
Death rates for COVID-19: Key issues, published data and what it tells us
Has the death rate of COVID-19 increased or decreased since May 2020? This article is an update from the previous analysis for the COVID-19 Blog on this issue.
|
The key findings from our analysis are:
|
Mortality by age
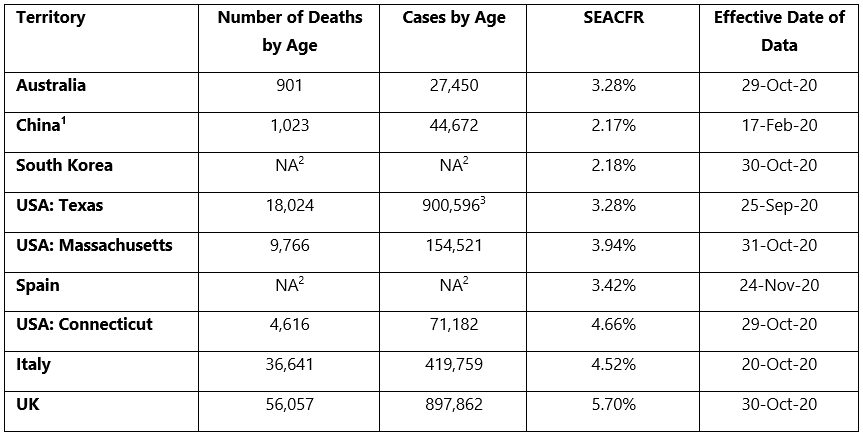
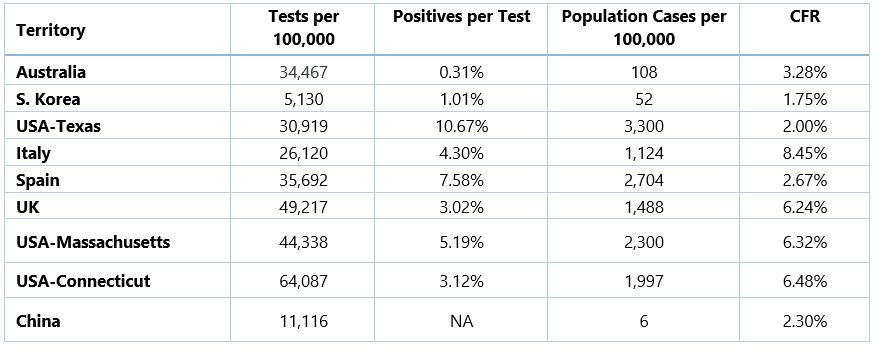
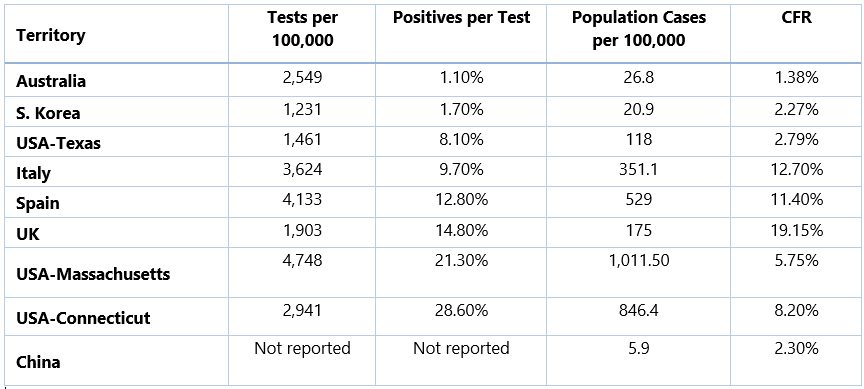
In May 2020, we have provided a summary of COVID-19 mortality, based on Standardised Equivalent Australian Case Fatality Rate (SEACFR) for different territories. With more data available since May 2020, we have updated the COVID-19 mortality table for those territories. The territories are listed below from lowest to highest COVID-19 mortality, based on a measure that we call Standardised Equivalent Australian Case Fatality Rate (SEACFR).
The SEACFR is the weighted average of a territory’s age-based Cate Fatality Rates (CFRs), with the weights based on Australia’s age-based reported infection profile i.e. it is indicative of a territory’s overall population CFR if its age profile for infections was similar to Australia.
|
1. There is no updated data for China, so the effective date of data is still as of February 2020 |
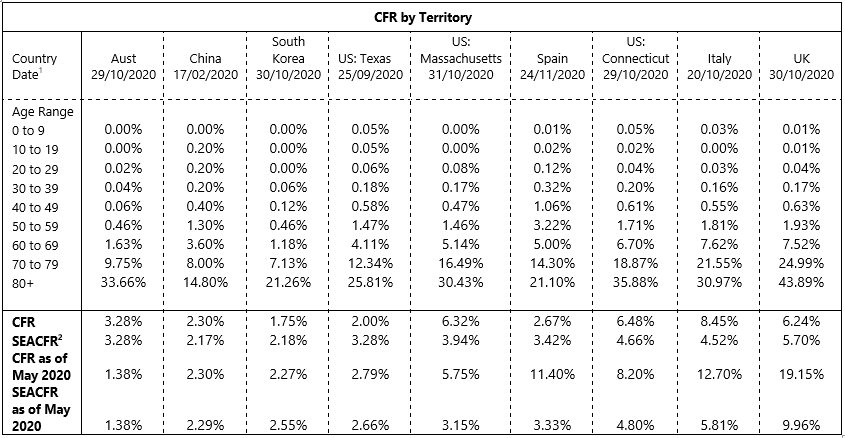
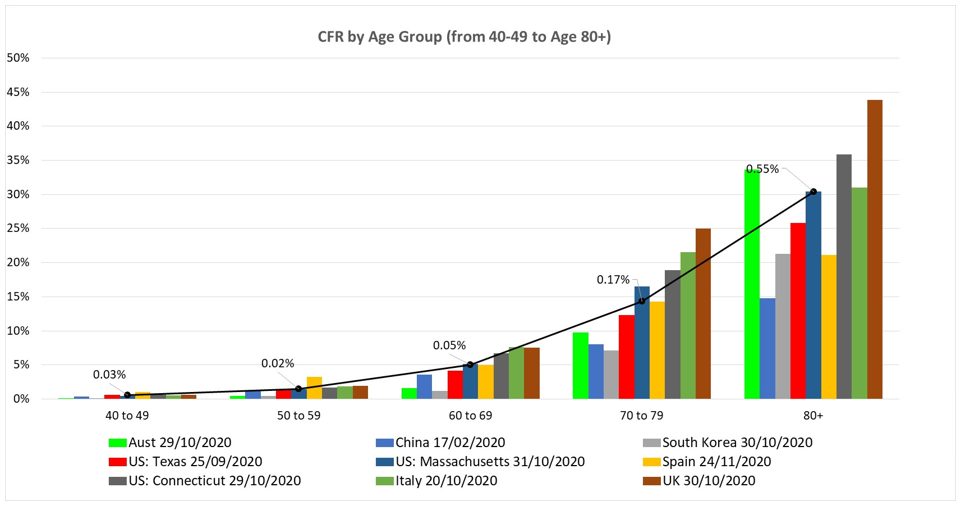
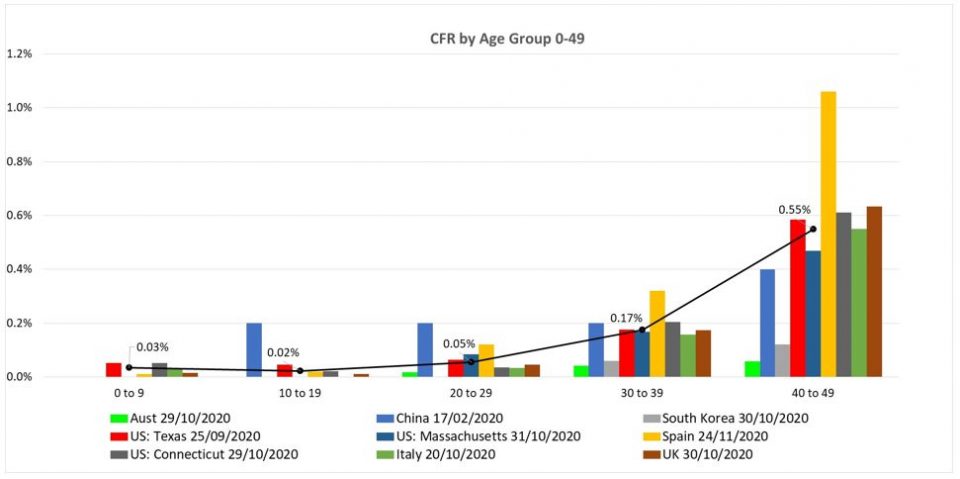
CFRs by age for each region are set out in the table and graphs below. The tables/graphs contain the same information with the following points noted.
- The graphs show the median CFR which is calculated separately for each age-group. For the younger ages the median calculation does not include countries which have a zero CFR.
- The first chart below shows age band from age 40-49 to age 80+. The second chart below shows ages 0-49.
|
1. Effective date of data – all dates 2020 |
Critical in interpreting this information is understanding countries’ ability to identify and report infections and deaths. All other things being equal, if infections are under-reported but deaths are not, the resultant CFR will be overstated. However, if deaths are also under-reported, the overstatement will reduce, and the measured CFR might even be understated.
All territories are likely to have under-reported infections in the first wave, when testing had to be rationed. Many may have also significantly under-reported deaths, especially when people died at home.
|
*Test data from 1 November 2020
|
The table as of May 2020 is also shown below for comparison purpose:
|
*Test data from 4 May 2020
|
Compared to May statistics, the following is observed:
- For Australia, overall CFR increased from 1.38% to 3.28%, mainly due to increases in infections and deaths in the age band 70-79 and age band 80+. This might be due to the higher number of infections in aged care settings in the second wave from July to August 2020. For US Massachusetts, there is a slight increase in CFR.
- The overall CFR for South Korea has not changed significantly and is only slightly dropped from 2.27% to 1.75%.
- For US Texas, US Connecticut, Spain, Italy and UK, the overall CFR has decreased compared to May 2020 statistics. This is also associated with the drop in ‘positives per test’. As we previously mentioned, we think that the high rate of positive testing may be one indicator of a higher level of ‘real’ cases not identified and ‘missing’ in the ‘reported’ infected numbers. For example, in May 2020, UK has a high positive per test rate of 14.8% and a relatively high CFR of 19.15%. In November 2020, the positive per test rate has dropped to 3.02% and the CFR has also decreased to 6.24%.
The following shows the infection rate per age group for the different territories. It suggests that the infection rate for younger age 20-29 and older age 80+ are higher.
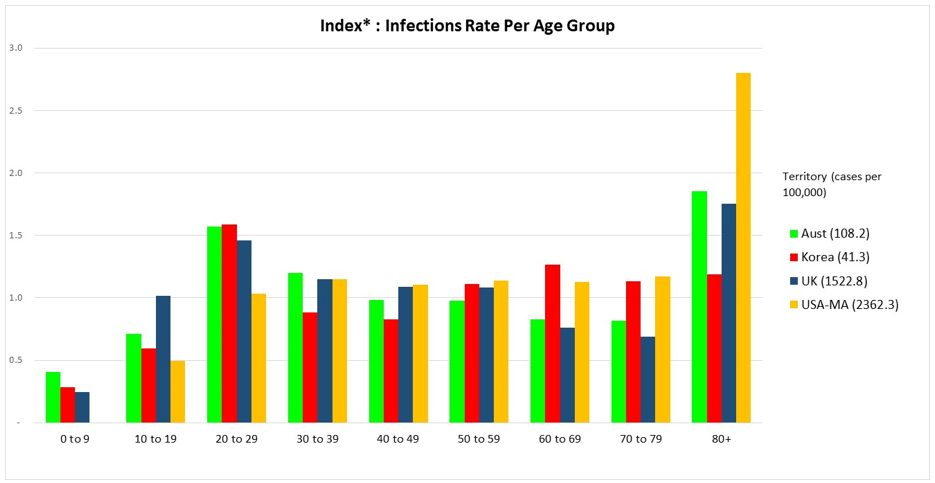
|
*A value of 1 means that for that age band, the infection rate is the same as the average for the whole population of that region. E.g. Australia has an average infection rate of 108.2 per 100,000 – the Index value for age 20-29 is 1.6, so the infection rate for that age band is 169 per 100,000 (1.6 x 108.2).
|
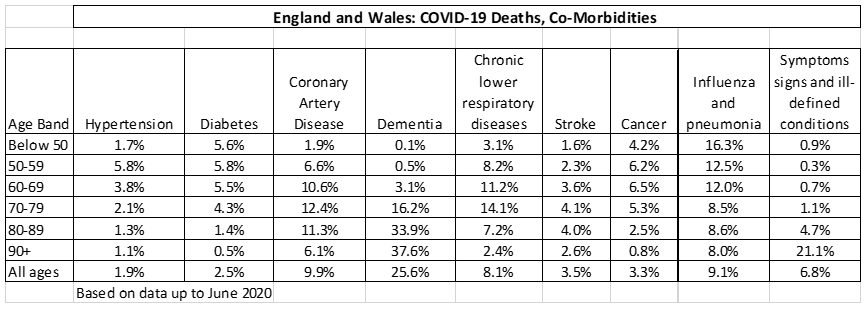
Co-Morbidities
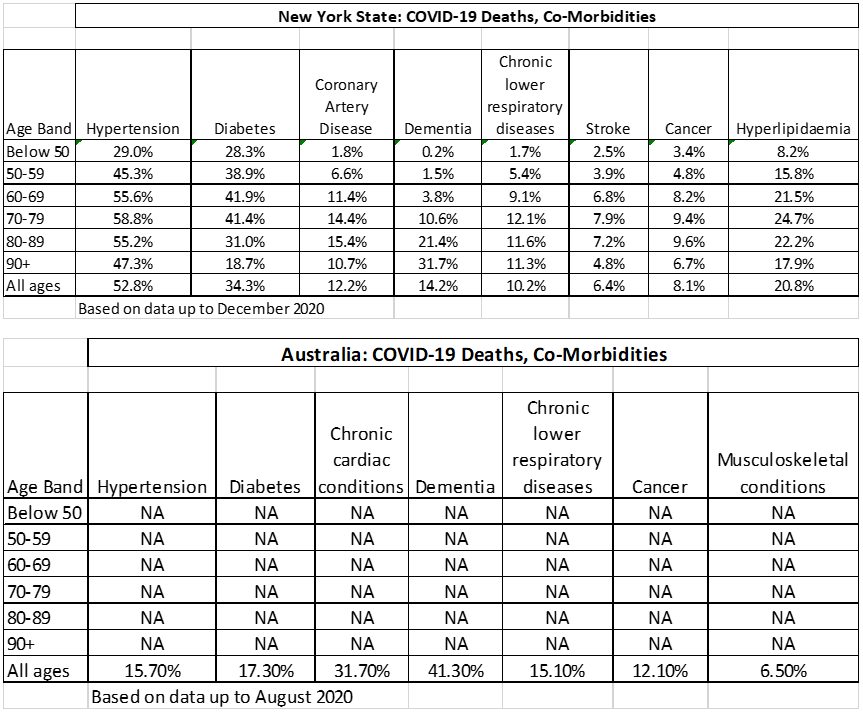
We analysed deaths involving COVID-19 by the pre-existing conditions for UK (England and Wales), New York State and Australia.
The following table shows the co-morbidities for England and Wales, New York state and Australia. For Australia, ABS provided the proportion of COVID-19 death with a pre-existing condition but not by age band.
|
England and Wales: http://bit.ly/3tqe1co New York State: https://on.ny.gov/3qNMLTy Australia: http://bit.ly/3eQCCTE |
The following graphs showed the top five co-morbidities of COVID-19 deaths for England and Wales, New York State and Australia. Note that the co-morbidities were working out based on COVID-19 deaths’ number of 100,670 (up to June 2020) for England and Wales, 29,789 (up to December 2020) for New York State and 683 (up to August 2020) for Australia respectively.
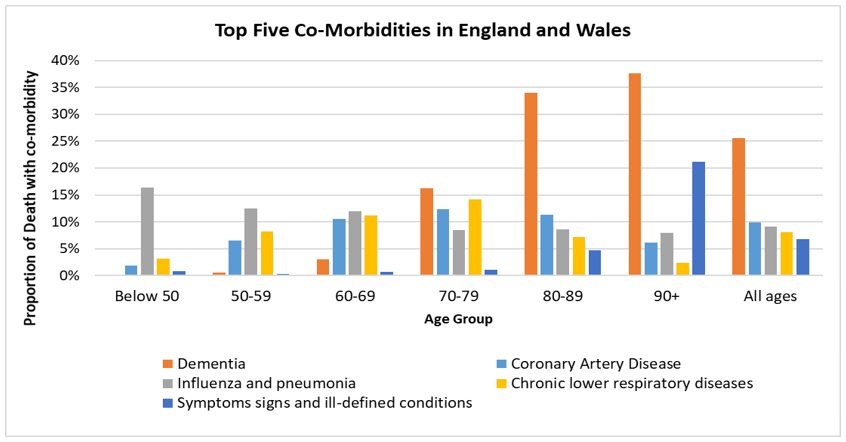
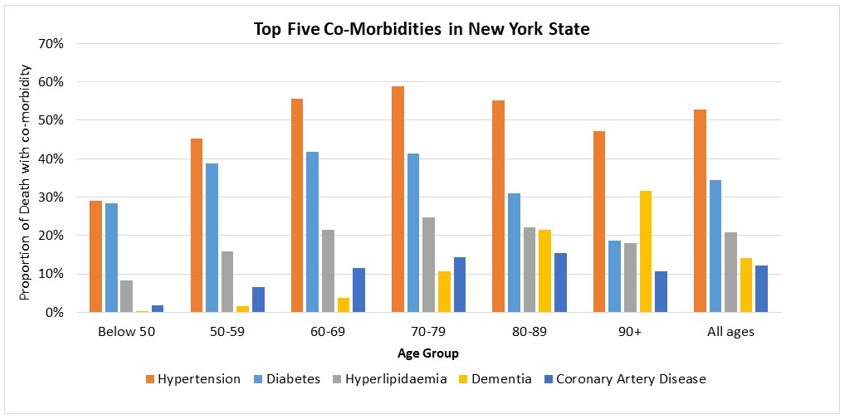
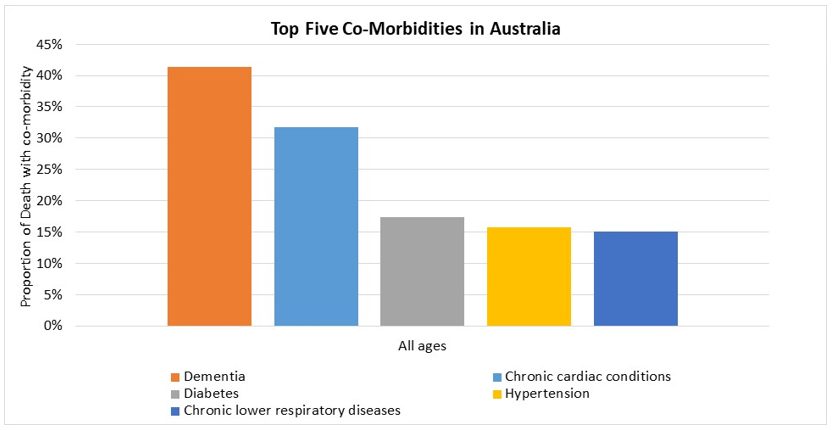
Dementia was the most common pre-existing health condition in COVID-19 deaths for England and Wales (25.6%), and Australia (41.3%). For England and Wales, as we can see from the graph above, Dementia was more prominent for the older ages from age 80+. Dementia was the fourth most common pre-existing health condition for New York State.
Coronary Artery Disease was the second common pre-existing health condition in COVID-19 deaths in England and Wales (9.9%). It has the proportion of 12.2% in New York State (fifth most common).
For hypertension, it was the most common pre-existing condition in New York State for COVID-19 deaths (52.8%). However, in England and Wales, the proportion of hypertension in COVID-19 deaths was only 1.9%.
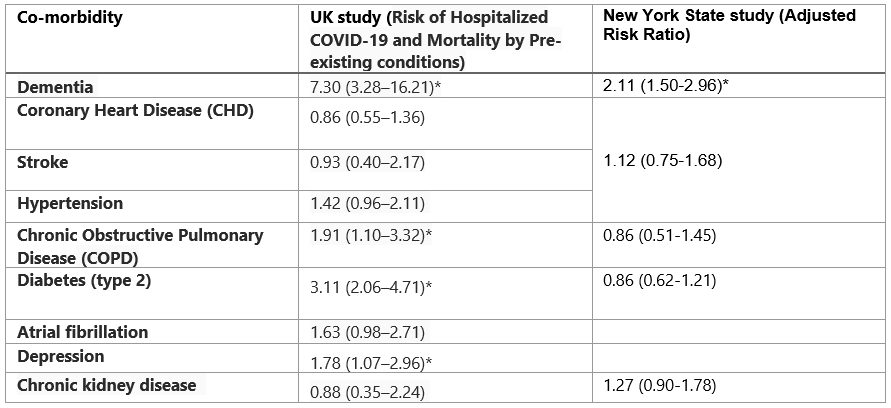
One of the UK (England) studies associations between pre-existing diagnoses and hospitalised COVID-19 with mortality, in a large community cohort. Similarly, another study was conducted based on COVID-19 statistics in New York State.
The following table shows the results from UK and New York state.
|
*Means P value is less than 0.05
|
As we can see from the above table, pre-existing dementia in both the UK and New York State study was associated with the largest risk increase and is statistically significant. Diabetes (type 2) was the second highest risk increase of death from COVID-19.
For hypertension, both UK and New York State study showed that hypertension pre-existing condition might increase the risk of death from COVID-19. However, hypertension in both studies did not reach a statistical significance for being COVID-19 and dying.
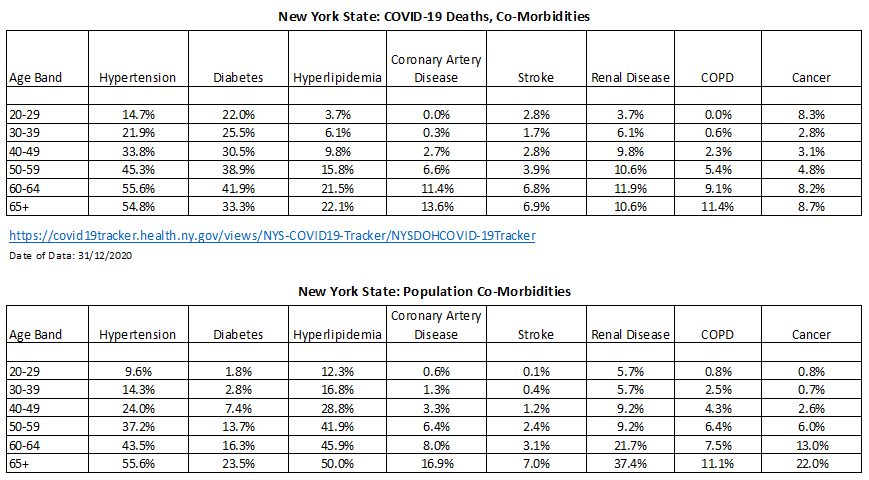
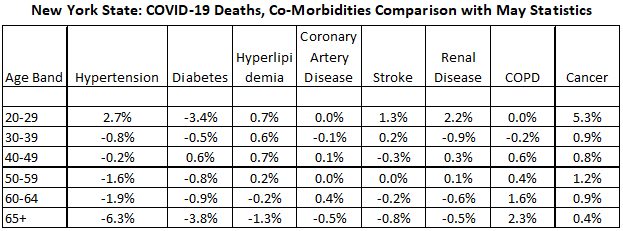
In May 2020, we compared rates amongst COVID-19 deaths for New York state with age-based rates of co-morbidities in the general population. With updated data in December 2020, we have updated the comparison table with updated COVID-19 deaths numbers. The following tables show the result. Overall, the co-morbidities within COVID-19 death have not changed significantly.
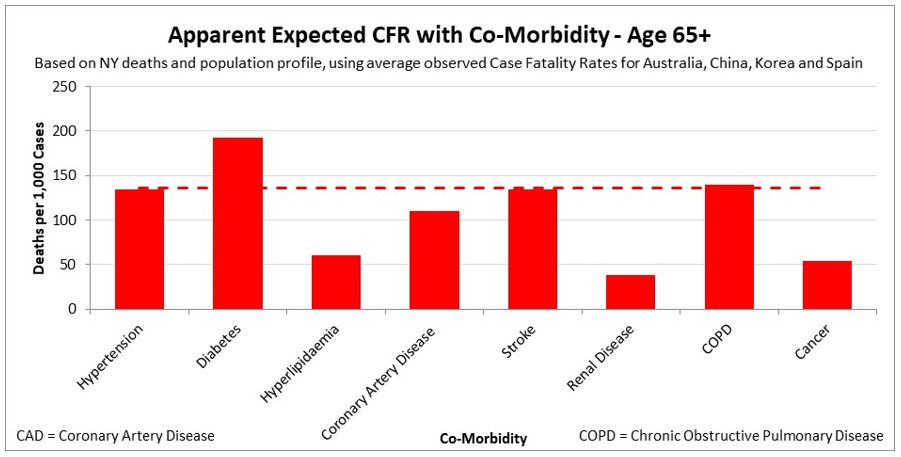
The following table gives ratios or multipliers to the presumed base level of COVID-19 mortality from the key co-morbidities. With the updated data, this still shows unexpected, and often low, co-morbidity outcomes, most notably for COPD, given COVID-19 is a respiratory disease. New York co-morbidity study also showed that the pulmonary conditions were not associated with higher mortality
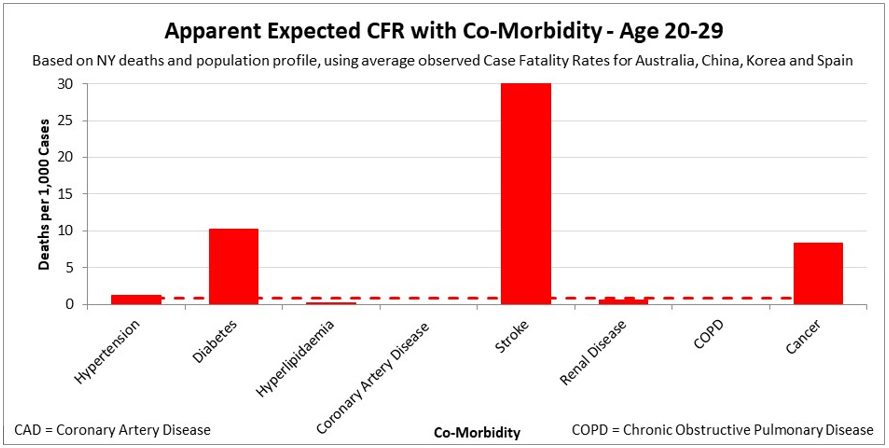
There appear to be, however, two highly significant co-morbidities for younger people, as shown in the table, diabetes and stroke.
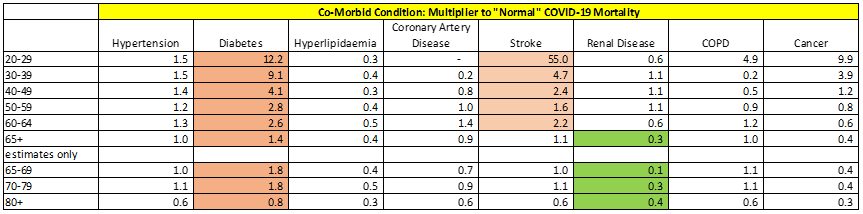
The results for diabetes and stroke are highlighted in the graphs below.

The result is consistent with the above UK co-morbidity study which suggests that Diabetes increases the risk of death from COVID-19 (the second highest increase across the co-morbidities considered).
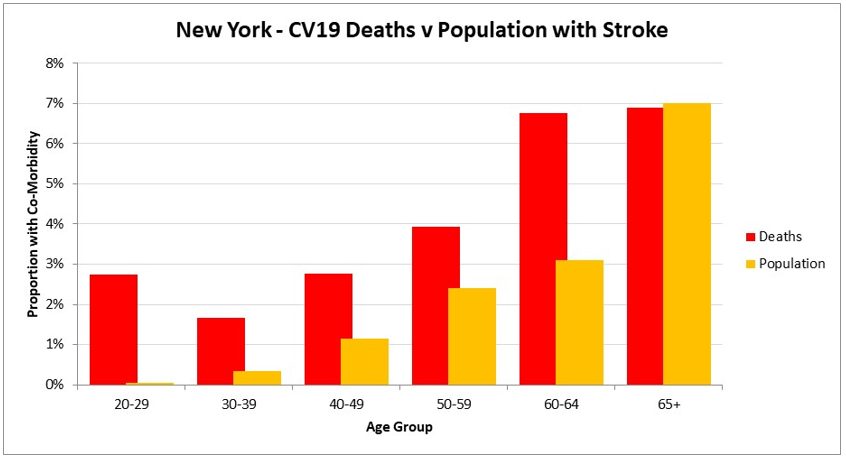
For stroke the New York co-morbidity study showed a slight trend towards higher mortality but the UK co-morbidity study was the other way around. However, both results were not considered statistically significant.
Given stroke can be a consequence of COVID-19, the high prevalence of it as a co-morbidity in COVID-19 deaths might point to an outcome instead of a risk factor. On the other hand, it is possible that COVID-19 might be more severe for those with a higher natural propensity for stroke. And it is not clear how we would identify such people in population data and COVID-19 deaths. Hence, it is difficult to make a conclusion from the current available data.
The following table and graphs show apparent expected CFR with co-morbidity:
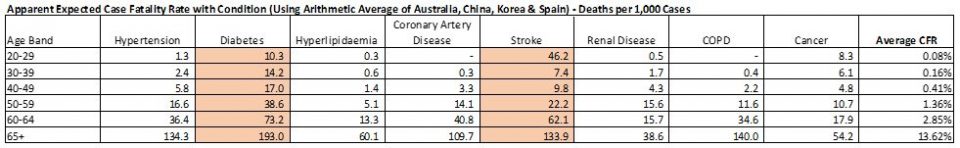
Apparent expected CFR for each co-morbidity is calculated based on New York State deaths and population profile, adjusted by average observed CFR for Australia, China, Korea and Spain.
CPD: Actuaries Institute Members can claim two CPD points for every hour of reading articles on Actuaries Digital.






