
Excess Mortality: Considerations in Moving Away from a Pre-pandemic Baseline
The Mortality Working Group is planning to make a significant change to the baseline (or expected number of deaths) used when measuring excess mortality for Australia.
The Working Group intends to move away from the philosophical question of “How has the pandemic affected mortality?” to instead answer the question “Is 2023 mortality the ‘new normal’?”
Purpose
The purpose of this article is to set out considerations for setting a baseline (or expected number of deaths) for use in excess mortality calculations for the year 2024 and beyond. Many of the finer details still need to be determined, but this article sets out the conceptual framework that the Mortality Working Group intends to adopt for measuring excess mortality in 2024.
Background
With the COVID-19 pandemic, there has been a huge amount of interest in excess mortality calculations – that is, estimates of the number of deaths over and above what would have been expected. To date, the bulk of these calculations, including ours, have used an expected number of deaths had the pandemic (COVID-19) not occurred. This has been an entirely appropriate way to estimate the baseline, and the resulting excess mortality is an estimate of the net mortality impact of the pandemic.
We are, however, now in the fifth year of COVID-19. This means that it is now several years since the population experienced pre-pandemic mortality. Extrapolations generally assume that pre-pandemic mortality trends would have continued, and it is debatable whether this is a valid assumption to hold for a five-year extrapolation period.
Consider, for example, the projected 2020 standardised death rate (SDR) based on linear trends of the five-year periods from 2011-2015 to 2015-2019. The projected 2020 SDR ranges from 504.3 (using 2015-19 as the base) to 534.6 (using 2013-17 as the base), a 6% difference, which is large in the context of measuring excess mortality.
It is also arguable that excess mortality calculations should no longer be trying to measure “the impact of the pandemic”. Alternative questions may be “How is current mortality tracking relative to pandemic years?” or “How is current mortality tracking relative to the last year?”
These questions may help determine whether we are now at a new normal level of mortality – i.e., is the 2023 mortality a reasonable starting point, or does it still include some pandemic-related “shocks” to mortality?
Clearly identifying what is meant by “excess mortality” will ultimately determine how to set the baseline.
New ONS methodology for calculating excess deaths
In February 2024, the UK’s Office for National Statistics released a methodology paper[1] setting out its new approach to measuring excess mortality. We are pleased to see that the ONS is moving to a methodology that allows for changes in both population size and age characteristics over time. The ONS has also decided to include pandemic years in the data used to set the baseline, however individual weeks and months with very high COVID-19 mortality[2] are removed.
This provides a communication challenge. While it is difficult to articulate, in our view the ONS has not clearly explained what the new baseline represents. Until now, most baselines (including those of the Mortality Working Group and the Australian Bureau of Statistics) have been expected deaths in the absence of the pandemic. The new ONS baseline is clearly not this, but what is it?
For 2024, the ONS baseline uses data from 2018-2023, covering:
- two pre-pandemic years, one of which happened to have unusually low mortality; and
- four pandemic years, excluding the two very high COVID-19 waves.
So, if 2024 results in no excess mortality, is this a good or a poor outcome?
We are not suggesting that this is a simple exercise but, at the same time, it seems somewhat unhelpful not to try to explain (in words) what the excess represents – the excess over and above what?
As time progresses, and the pandemic impact on mortality becomes a historical fact, this will become irrelevant. However, at the stage we are at now, having a mix of pre-pandemic and pandemic years used to determine the baseline is not easy to explain nor understand.
Estimate of including pandemic years for Australia
We have formed a fairly rough-and-ready estimate of the baseline for 2024 if we included pandemic years when setting the baseline. We have estimated the expected number of deaths in 2024 by fitting a linear trend to deaths from 2017 to 2023 (i.e., seven years of data). Our estimate here is very approximate and is provided as an indicative estimate only.
Using data to 31 December 2023, we estimate that total deaths in 2023 may be around 183,700 (after including a small allowance for late-reported deaths). If we include pandemic years in setting the 2024 baseline, the expected number of deaths in 2024 might be, roughly, around 190,000.
Figure 1 – 2024 baseline if pandemic years included
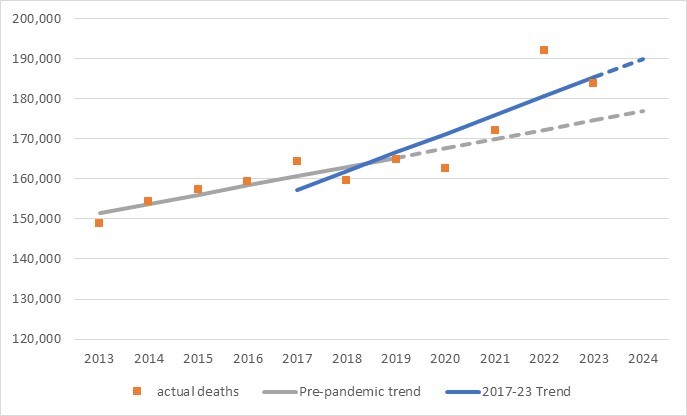
Based on what we know about the causes of mortality in 2022 and 2023, we think that this is an unrealistically high expected number of deaths. The mechanistic inclusion of data from pandemic years into the model does not produce a realistic estimate of the expected number of deaths. Even if some of the pandemic spikes in mortality were excluded, we expect that the application of the model would still produce an unrealistically high estimate of mortality for 2024.
As for the discussion of the ONS baseline, our key question is, what does the measured excess mortality mean? Would negative excess mortality in 2024 against the mechanistic seven-year trend convey the right message about 2024’s mortality?
What might a reasonable baseline for 2024 look like?
The following table is taken from our analysis of excess mortality to 31 December 2023. It shows the estimated excess broken down by cause of death for each of the pandemic years. Note that the excess is measured relative to pre-pandemic expectations of mortality and that these expectations build in the mortality trend for each cause.
Table 1 – Excess mortality by cause of death – 2020 to 2023
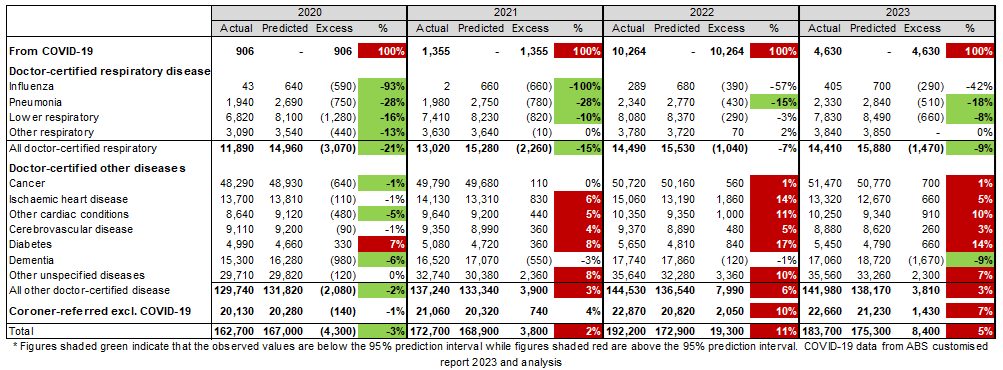
The table shows that:
- COVID-19 deaths are significantly lower in 2023 compared with 2022. There is a high degree of uncertainty surrounding any predictions of COVID-19 deaths as they will depend on the number of COVID-19 waves, the severity of any new strains, the level of both vaccine- and infection-induced immunity in the community, etc. However, unless there is a severe new strain, it seems likely that the number of COVID-19 deaths in 2024 will be lower than the number in 2023, as each wave is producing fewer deaths;
- deaths from other respiratory diseases and dementia were significantly lower than expected in 2023, most likely due to the use of masks and other NPIs in aged care and hospital settings. As some defence measures remain in place, it is likely that the number of other respiratory deaths will continue to be lower than pre-pandemic expectations in 2024;
- cancer deaths make up around 30% of all deaths, and cancer mortality has been largely unaffected by the pandemic; and
- deaths from all other causes were significantly higher than expected in 2022 and 2023, but the level of the excess in 2023 was lower than in 2022 for all causes.
In our view, a reasonable estimate of a baseline for 2024 would:
- take the 2023 age-standardised rates of mortality, by cause of death, as a starting point;
- for deaths due to COVID-19, adopt age-standardised mortality rates for 2024 that allow for two waves per annum (as we have seen in the last 18 months or so), with each successive wave resulting in fewer deaths than the previous wave, reflecting the trend that we have seen since borders were re-opened;
- for respiratory causes, adopt the 2023 age-standardised mortality rates for 2024. Due to the nature of respiratory diseases, it is reasonable not to allow for any mortality trend; and
- for all other causes of death, adopt the 2023 age-standardised mortality rates plus an allowance for the pre-pandemic rate of mortality improvement to continue into 2024.
Illustrative example
We have applied this approach to the available data, noting that the figures shown here are indicative only; we have used simplified modelling techniques to illustrate the concept[3].
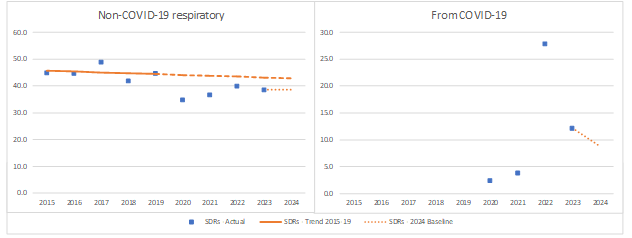
The following graphs show for each non-respiratory, non-COVID-19 cause of death:
- actual SDRs (blue dots);
- the pre-pandemic trend line using a linear trend based on 2015-19; and
- the application of the same trend line to the 2023 actual SDR – other models (i.e. non-linear) and different data periods may be more suitable.
Figure 2 – Indicative 2024 baselines by cause of death – Non-respiratory, non-COVID-19

The following graphs show the same information for non-COVID-19 respiratory deaths and deaths from COVID-19. For the 2024 baseline, no mortality trend is assumed for respiratory deaths. For COVID-19 deaths, the 2024 baseline assumes two COVID-19 waves, each resulting in 15% less deaths than the previous wave (noting that the assumption of a 15% reduction per wave is indicative and our final assumption may differ from this).
Figure 3 – Indicative 2024 baselines by cause of death – Respiratory and COVID-19
The following graph shows the resulting all-cause SDRs.
Figure 4 – Indicative 2024 baseline – All Cause
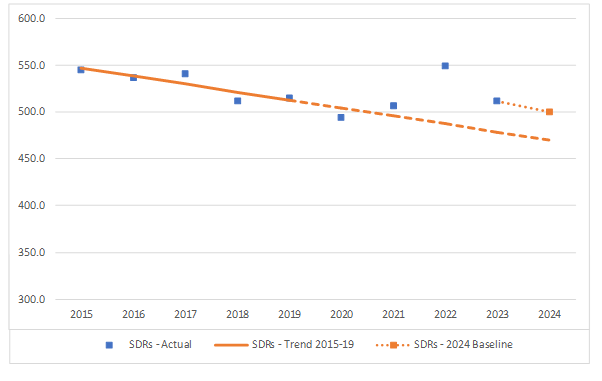
This indicative modelling results in an all-cause baseline SDR for 2024 that is similar to the actual SDRs for 2020 and 2021.
Framing the measured 2024 excess mortality
The excess mortality question posed by the suggested baseline may be:
“How does 2024 mortality compare to the expected level based on 2023, after making allowance for reasonable expectations for mortality improvement?”
Or, more simply: “Is 2023 mortality the new normal?”
We acknowledge that:
- there are most likely still temporary pandemic impacts included in 2023 mortality;
- these temporary pandemic impacts are impossible to quantify;
- there is an expectation that underlying non-COVID-19 mortality will continue to improve, as it has done for decades prior to the pandemic;
- it is unclear whether the underlying mortality improvement rate would, by now, be higher or lower than the pre-pandemic trend; and
- therefore, there is more than usual uncertainty around the appropriate baseline for expected mortality and this uncertainty will continue as we move towards new normal post-pandemic mortality.
We stress the high uncertainty (and wide confidence interval) relating to the resultant calculation of excess mortality.
Baseline for 2025 and later years
While it is early to be thinking about a baseline for 2025 and later years, we wanted to make it clear that our adopted framework for the 2024 baseline applies to that year only.
We envisage that, as time progresses, the baseline would evolve and more post-2022 years would be included in setting the baseline.
Our current thinking is that:
- for the 2024 baseline, the pre-pandemic trend is the only option we have for non-COVID-19 mortality improvement, while the 2023 experience is our only credible data point;
- for the 2031 baseline, we would expect to use both data and mortality trend derived from the 2023-2029 experience (i.e., reverting to a seven-year modelled period), with pre-pandemic trends finally consigned to history; and
- in the intervening years, a credibility-based approach could be used to give more or less weight to pre- and post-pandemic experience, such that the baseline moves seamlessly from the suggested 2024 baseline to the 2031 baseline.
The implementation of this idea will need further thought and development. It is reasonable to suppose that elements will change, depending on the actual mortality experience that emerges in the next couple of years.
Mortality Working Group
The members of the Working Group are:
- Karen Cutter
- Ronald Lai
- Jennifer Lang
- Han Li
- Richard Lyon
- Matt Ralph
- Amitoze Singh
- Michael Seymour
- Zhan Wang
References
[1]https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/causesofdeath/articles/estimatingexcessdeathsintheukmethodologychanges/february2024
[2] Defined as where more than 15% of all deaths are from COVID-19
[3] Deaths from COVID-19 shown here include an estimate of coroner-referred deaths from COVID-19 (which are in turn deducted from the coroner-referred deaths).
CPD: Actuaries Institute Members can claim two CPD points for every hour of reading articles on Actuaries Digital.






