
An Introduction to Value-Based Care and the Potential Role of Actuaries
Learn about the transformative potential of Value-Based Care in addressing Australia’s healthcare challenges through improved outcomes and cost management.
Contents
Executive summary
The Actuaries Institute’s Health Practice Committee established a Working Group to examine how actuaries can contribute meaningfully to Value-Based Care (VBC), an approach that aims to address Australia’s healthcare challenges by improving health outcomes while managing costs.
VBC encompasses four key components: transparency in delivery and outcomes, quality of care, patient/family experiences, and value for money, requiring integrated healthcare teams to work collaboratively in addressing patients’ shared health needs.
Our analysis reveals three significant barriers to broader VBC adoption in Australia:
- non-uniform definitions of health issues and outcomes;
- technological challenges in data sharing and analysis; and
- funding model complexities.
Drawing on successful examples from the Netherlands and Sweden, we demonstrate how these barriers can be overcome through robust frameworks for measuring outcomes and sustainable funding models. These programs have achieved significant improvements in both clinical outcomes and costs, including a 15% reduction in reoperation rates for breast cancer care and 20% reduction in complications for joint surgery.
Actuaries have a core role to play, alongside other professionals, to facilitate the uptake of VBC in Australia. Data, analysis, risk and benefit quantification, reliable reporting and forecasting are all core actuarial skills and will be important for each key component of VBC, and in addressing the barriers.
Introduction
Australia’s health system faces challenges in relation to rising costs, profitability, capacity constraints, and how services will meet the needs of an aging populations in the future. The system is complex, with many healthcare providers and many ways in which healthcare in Australia is funded. Interactions between private and public healthcare service delivery add to this complexity.
Within the system, each stakeholder has individual needs and expectations which are sometimes aligned and sometimes disparate. Balancing these needs and expectations is important to have a sustainable system for all stakeholders to meet these challenges in the future.
Many potential courses of action are available to try and meet these challenges, one of which may be Value-Based Care (VBC).
The Actuaries Institute’s Health Practice Committee established a working group to look into how actuaries can make a meaningful contribution to value-based care. While actuaries have worked alongside healthcare professionals for many years they do not have a long working history in value-based care.
This article aims to inform and engage the actuarial community on value-based care and its potential impact in transforming Australia’s health ecosystem. The working group has explored various dimensions of value-based care, including what it is, how it is considered by different stakeholders, barriers to its implementation, and lessons learned from other jurisdictions. These are summarised in this article.
An overview of the health ecosystem in Australia
Australia’s healthcare system is a complex network of private and public providers and stakeholders, each playing a critical role. Key stakeholders include:
- Australia’s State and Federal Governments: These bodies are responsible for funding, regulating, defining, and managing the nation’s health system.
- Healthcare providers: This group encompasses public, for-profit, and not-for-profit organisations, including general practitioners (GPs), specialist doctors, and other care providers, all tasked with delivering healthcare services.
- Patients and families: These individuals navigate the healthcare system to receive care, often bearing out-of-pocket costs for services.
- Private health insurers and Medicare: These entities fund various treatments.
- Regulators and health associations: These organisations define best practices and ensure compliance with laws and policies.
The healthcare system’s structure is underpinned by the division of responsibilities and funding among Federal and State governments and private entities. This distribution is illustrated in the chart provided by the Australian Institute of Health and Welfare.
Figure 1: Funding and responsibilities of health services in Australia
We see:
- The complexity of funding arrangements and the division of responsibilities can be confusing to external observers.
- The health industry comprises numerous public and private providers, which predominantly operate independently.
Actuaries have been integral to Australia’s health insurance industry for decades, aiding insurers, healthcare providers, funders, and regulators in understanding the implications of their decisions on the costs and health outcomes of Australians.
Australia’s aging population, the increase in chronic health conditions, high-cost and high value technology advancements, and the need for strategic long-term financial planning are challenges that will require system-wide solutions to address. Actuaries are well-positioned to contribute significantly to these collaborative efforts in the future.
What is Value-Based Care?
Understanding value in healthcare
In the health industry, value is fundamentally about maximising health outcomes while minimising costs. This principle underpins the implementation of Value-Based Care (VBC), a concept familiar to the Healthcare sector. Despite its longstanding presence, achieving the right balance remains challenging due to the complex array of health outcomes, evolving technology for care delivery, changing stakeholder expectations and rising costs.
Stakeholders generally agree on two points:
- Care pathways should lead to, or be expected to lead to, improved health outcomes for individuals.
- Costs, both financial and non-financial, are considered. Noting costs should not be the sole determinant of the nature, timing, and method of medical treatment.
There is consensus that both health outcomes and costs should be measured and reported in an appropriate forum. Data should capture both patient health improvements and healthcare costs.
Challenges in Value-Based Care
Beyond these initial agreements, VBC presents challenges including:
- Defining and measuring improved health outcomes.
- Defining and collecting cost data.
These concepts vary significantly among stakeholders. Opinions differ in relation to maximising ‘value’ and determining which health outcomes justify their associated costs. Data collection, storage, and privacy also pose significant challenges, further hindering measuring outcomes and VBC progress.
Stakeholder perspectives on Value-Based Care
To understand the diverse perspectives, we examine stakeholder expectations and what health outcomes and costs mean to them:
- Patients and Families: Patients’ focus is on managing or resolving their specific health issues, often expecting seamless care from a single provider. However, patients frequently require multiple health care providers, relying on referrals for positive outcomes.
- Healthcare Providers: Healthcare providers aim to address patient health outcomes efficiently. They face increasing cost pressures as healthcare expenses rise, surpassing funding and GDP growth, squeezing profit margins.
- Healthcare Funders: Healthcare funders, where they have control, work with providers and regulators to assist their members or themselves to achieve desired outcomes effectively. This helps achieve as low as possible premiums and government budget impacts. However, disparities in outcomes and cost pressures have led to reduced health insurance coverage and increased patient out-of-pocket expenses.
- Regulators: Regulators oversee the market in a method which supports participants, using bespoke metrics for health outcomes. They set targets for these metrics and monitor providers against these to support the users of the services provided, be them in a hospital setting or from an insurer.
Industry group perspectives
Key themes emerge when reviewing how VBC is considered by health stakeholders:
- There is no consensus on whether effectiveness is just about service delivery or whether it includes metrics such as outcome measures, safety and quality.
- Some organisations, like private health insurers, have begun collecting effectiveness data (e.g., Patient Report Experience Measures and Patient Reported Outcome Measures) but have yet to integrate these into financial contracts.
- Few formal policy positions and action plans exist in Australia. While many industry bodies are considering VBC, few have published detailed actions or experiences.
There are several factors to consider when examining ‘health outcomes’ and ‘costs’ under the VBC lens, noting the list below is non-exhaustive:
- Patient health factors such as health improvement or likely health improvement, discomfort, health risks and complications
- Patient experience factors such as accessibility, timeliness of services, privacy, quality of food
- Factors related to the episode of care such as time in hospital, delivery model (integrated care teams), recovery time, setting of the care
- Financial factors including payments by the patient, insurer or Government, profitability of procedure and cost efficiency of procedure
- Post-care factors related to time out of work force or away from normal societal activities.
Aligning the definition of Value-Based Care
Most stakeholders agree that VBC centres on improving health outcomes through robust service delivery, encompassing overall care quality, patient and family experiences, transparency, and efficiency. However, differing views on the balance of the improvements between providers and funders can create an impasse, making a single VBC definition elusive. Considering all views and expected actuarial involvement in VBC, we propose Value-Based Care is defined with four components:
- Transparency
- Quality of care
- Patient/Family experiences
- Cost of delivery
In this framework, VBC includes the comprehensive experiences of patients, their families, and healthcare staff.
A framework for Value-Based Care
Having established the healthcare ecosystem, the interests of various stakeholder groups, and a shared understanding of Value-Based Care (VBC), we revisit our definition and compare it against recognised formal models including Michael Porter and Elizabeth Teisberg where the framework for implementing VBC consists of five key steps. Other academic literature on VBC includes similar components, which align broadly with the framework we propose.
Figure 2: Strategic framework for value-based health care implementation to achieve better patient outcomes
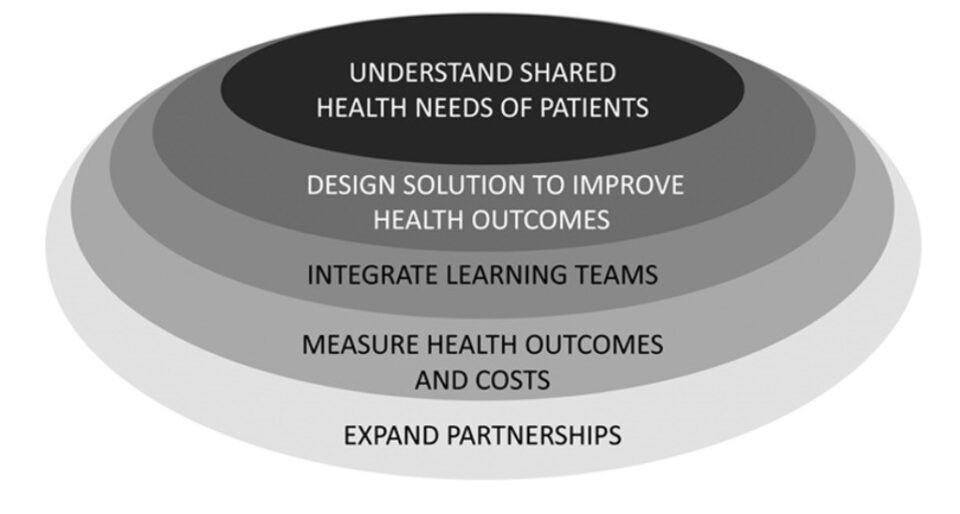
These steps are outlined as follows:
- Understand shared health needs of patients
VBC is most effective when patients with similar health needs are identified and grouped together, allowing for efficient delivery of commonly required services by integrated care teams and consistent measurement of health outcomes. Examples include groups such as “people with knee pain” or “elderly individuals with common chronic conditions.” - Design solutions with integrated teams
Ideally, VBC solutions should be designed around patients’ shared needs and delivered by integrated, multidisciplinary teams. For instance, physiotherapists and orthopedic surgeons may collaborate with other providers to provide care for individuals with knee pain. For some groups, health-adjacent services such as counseling and transportation assistance could be included. - Measure health outcomes and costs
Measuring health outcomes and delivery costs is essential to improve health outcomes and efficiency. Key components include patient-reported outcome and experience measures relevant to each group, which should be considered alongside other metrics, such as readmission rates. - Expand partnerships
VBC implementation typically begins locally, with a few providers collaborating to enhance health outcomes and efficiency for specific patient groups in pilot programs. As data is collected and improvements are demonstrated, these programs can be expanded by incorporating additional providers or applying lessons to new VBC initiatives for different patient groups. The greater the scale of VBC, the more opportunities there are for efficiency and health outcome improvements. Funders and providers can collaborate further to promote and share the benefits of enhanced outcomes and efficiency.
Barriers to implement Value-Based Care
If Value-Based Care (VBC) is seen as a key strategy to address the needs of various stakeholders, why it is not yet the standard approach to healthcare delivery? While some countries have made notable strides in adopting a VBC framework, Australia has not progressed as far. We identify three primary barriers to broader adoption:
- Lack of uniform definitions for health issues and outcome measures.
- Technological challenges.
- Funding challenges.
Non-uniform definitions and outcome measures
Ideally, patients would be grouped based on similar needs, allowing well-defined, integrated, multidisciplinary teams to address these needs. In reality, patients’ needs can vary significantly due to personal circumstances and other stakeholders’ differing opinions.
In a value-based care environment, a third-party care manager coordinates and provides included services to the patient. However, without a standardised approach to defining health issues, these teams must establish their own pathways. While this can offer flexibility to cater to individual needs, it can lead to systemic inefficiencies. Without consistent outcome measures and a clear method for evaluation, there is no feedback loop to support continuous improvement.
Technological challenges
Understanding patients’ shared health needs and designing solutions with integrated teams require technology systems that can effectively store and access patient medical histories. Currently, different healthcare organisations operate with separate systems, making it difficult to collect, aggregate, and analyse patient data.
Another challenge is the ability, security, and willingness to share information across the industry and among providers. Even if individual systems function well, measuring health outcomes and delivery costs requires systems to share information transparently and instantly between patients and medical providers. Once technological, legal, and other considerations are addressed, advanced analytical skills, such as those possessed by actuaries, are needed to interpret the data.
Funding challenges
Funding remains a significant challenge to value-based care. The fragmented way in which healthcare providers are funded means there is insufficient incentive to create programs that may incur costs in one part of the system but benefit another. This is compounded by existing budget and cost constraints faced by many providers.
Implementing VBC often requires substantial investment in health IT, data collection, and analytics systems, even before considering infrastructure, personnel, and other costs associated with new care models. From an investment perspective, providers may hesitate to invest in infrastructure if they are uncertain about the return on investment or if economic incentives (e.g., bundled payment rates, outcome bonuses) are not aligned with their operational costs.
It remains unclear who should fund VBC models and how to create contracts and structures that satisfy all parties involved.
Other barriers
While we focus on three main barriers, many others exist, such as resistance to change, lack of health literacy among patients, and difficulties in accessing appropriate services for those living in rural areas.
Lessons from other jurisdictions
While Australia faces barriers to implementing Value-Based Care, other countries have made notable progress in this area. The healthcare systems in the UK, Netherlands, US, and Sweden offer valuable lessons for Australia, particularly in the realms of data management and funding. These are all areas of great interest to actuaries.
In the UK, the National Health Service (NHS) launched NHS RightCare to enhance healthcare value and address variations in outcomes through its “proven approach”. The three pillars of RightCare are:
- Intelligence – diagnosing issues and identifying opportunities.
- Innovation – developing solutions and guidance.
- Implementation – delivering improvements for patients and the population.
RightCare has faced criticism for its “proven approach”, as some argue that the quality and use of data need further substantiation.
The Netherlands has demonstrated positive outcomes from its value-based care program. Five care types across seven Dutch hospitals were selected as candidates for a VBC framework. Breast cancer care was the first to mature under this framework, resulting in a reduction in lumpectomy reoperation rates by over 15%.
The other four care types are progressing, utilising lessons learned from breast cancer treatment. The success in the Netherlands, founded on data, benchmarking, and model governance, stands in contrast to the UK experience and underscores the importance of these elements for VBC proponents in Australia, aligning well with actuarial expertise and the control cycle.
In the US, the Centers for Medicare and Medicaid Services (CMS) conducts pilot programs linking provider compensation to performance against quality measures. Examples include the “End-Stage Renal Disease Quality Incentive Program” and the “Hospital Value-Based Purchasing Program.” Additionally, the Vermont All-Payer ACO Model (VTAPM), in collaboration with CMS, aims for statewide health outcome improvements. Evaluations suggest positive shifts in utilisation, spending, and health goals, alongside a cultural shift towards value-based payment systems.
Despite 93% of surveyed healthcare organisations engaging in some form of value-based program1, operational barriers remain. Achieving the CMS goal of enrolling all traditional Medicare recipients in an Accountable Care Organization (ACO) by 2030 will require collaboration among payers, providers, and government. Current incentives may be inadequate; for instance, the Medical Group Management Association reported that 87% of physicians in the Merit-based Incentive Payment System found reporting costs exceeded payment adjustments received.
Sweden is a leader in VBC, having implemented an outcome-based payment system across its 21 regions for specific care types. Implementation occurs primarily through regional agreements with county councils. Sweden’s healthcare system benefits from extensive quality-based registries that provide quality indicators for assessing healthcare delivery. Multiple regions in Sweden use “bundled payment systems,” compensating providers for complete episodes of care, which holds them accountable for the care cycle, including complications. Compensation is adjusted based on patients’ preconditions and expected costs, emphasising provider accountability.
An example from Sweden is “OrthoChoice,” which uses a bundled payment system for hip and knee surgery. In this program, 3.2% of providers’ compensation was withheld and paid at year-end, contingent on meeting pre-established quality outcomes. This approach led to a reduction of approximately 20% in complications and revisions compared to a traditional reimbursement plan, with average total costs per patient decreasing by approximately 17%.
The US and Swedish models highlight the effectiveness of incentives. While Australia’s health funding models are mature, they are fragmented. Rebuilding these models to incentivise value-based care requires a targeted approach, similar to those in the Netherlands and Sweden, with a focusing on those care areas more suitable to VBC.
Actuaries and Value-Based Care
Central to Value-Based Care is the effective use of data, positioning actuaries as key contributors to its implementation. This requires a deep understanding of data, including defining terms, identifying underlying components, detecting biases, and ensuring data fitness for purpose. Monitoring the impacts and successes of initiatives can be invaluable for VBC.
The actuarial profession’s reputation for being objective, data-driven, unbiased, and transparent further enhances opportunities for actuaries in VBC. In a landscape with diverse stakeholders and potentially conflicting objectives, having independent, qualified, and credible professionals involved in implementation can lead to success.
Actuaries have had success in related fields already, working with Governments in Australia and internationally on the Priority Investment Approach, utilising modelling of future welfare outcomes to define what may be the most effective policy decisions to implement.
The competencies that are critical to define and measure VBC are central to the actuarial skill set. Specifically, actuaries are well-positioned to:
- Evaluate the financial implications and predict outcomes of strategic choices as care models evolve, providing rigorous analysis to define potential impacts.
- Use data to align actions with desired future outcomes, assisting to develop tools and metrics to measure and report on value and performance. This includes assessing performance at contract, provider, and service line levels by analysing future events and their potential costs.
- Identify and advise on risks, particularly financial, associated with VBC and develop risk management strategies.
- Collaborate with contracting teams to define contract terms and price them to optimise outcomes, drawing on pricing expertise from other areas to develop VBC contract methodologies.
Among international actuarial institutes and societies, the Society of Actuaries (SOA) in the United States has undertaken significant work in the field of VBC. Since 2020, the SOA has published a series of articles on this topic. Recognising the varied definitions of VBC, the SOA defines it as enhancing the patient experience, reducing per-capita medical spending, and improving population health. It focuses on the provider perspective and the role actuaries can play in enterprise and financial risk management.
Closing remarks
Value-Based Care (VBC) offers a method to meet current health challenges such as rising costs and an aging population by focusing on improving health outcomes while managing costs.
Actuaries, with their analytical and data skills, are well-suited to support VBC implementation through defining key terms, ensuring data quality, and evaluating financial implications. Our expertise in predicting outcomes and developing risk management strategies aligns with VBC goals.
International models from the Netherlands and Sweden provide valuable insights and demonstrate what can be achieved, particularly in data management, modelling and funding models. These examples underscore the importance of incentives and integrated care pathways, areas where actuaries can significantly contribute.
We hope the work here will provide a foundation and encourage actuaries to engage and help shape the future of healthcare delivery in Australia, either through engagement with VBC or other modes. The Institute’s HPC intends to continue exploring this area, welcoming any input from membership to either inform our direction or contribute to the working group.
References
CPD: Actuaries Institute Members can claim two CPD points for every hour of reading articles on Actuaries Digital.






