COVID-19 Mortality Working Group: Excess mortality continues in August 2022
Catch up on the Actuaries Institute’s COVID-19 Mortality Working Group’s latest analysis of excess deaths.
In summary:
|
Background
The COVID-19 Mortality Working Group has examined the latest Provisional Mortality Statistics, covering deaths occurring prior to 31 August 2022 and registered by 31 October 2022, released by the Australian Bureau of Statistics (ABS) on 25 November. This release also included the article COVID-19 Mortality in Australia, with details on all COVID-19 deaths occurring and registered by 31 October 2022.
Throughout this article we separate COVID-19 deaths into:
- Deaths “from COVID-19”, namely deaths where COVID-19 is listed as the primary/underlying cause of death; and
- Deaths “with COVID-19”, namely deaths where the underlying cause of death has been determined as something other than COVID-19, but the virus was a contributing factor.
This terminology is consistent with that used by the ABS and reflects the data provided.
In this article, we calculate excess deaths by comparing observed deaths to our ‘baseline‘ predicted number of deaths for doctor-certified deaths (by cause) and coroner-referred deaths (for all causes combined).
The Working Group has also examined excess mortality by age/gender and by state/territory. In so doing, we have used additional data from the ABS in relation to COVID-19 deaths registered by 30 September 2022, namely:
- The number of deaths each week both from COVID-19 and with COVID-19, broken down by age/gender; and
- The number of deaths from COVID-19 broken down by state/territory, noting that no information is available for deaths with COVID-19 broken down by state.
The age/gender data referred to above was provided to us privately by the ABS, while the state data comes from the ABS article COVID-19 Mortality by wave published on 16 November 2022.
We also provide an indicative estimate of excess mortality due to deaths from COVID-19 only, for the three months subsequent to the ABS data (September to November 2022).
Baseline Prediction by Cause of Death
Our previous Actuaries Digital article discussed in some detail how we arrived at our baseline predicted deaths. In short, our baselines are set by extrapolating linear regression models fitted to Standardised Death Rates (SDRs), which are then re-expressed as numbers of deaths. For the pandemic years, we have included different years to train the regression models:
- For 2020 and 2021, we have used the 2015-19 experience.
- For 2022, we have:
- used 2015-19 experience to set our baseline for deaths from respiratory disease and dementia, on the basis that 2020 and 2021 experience for these causes was materially affected by the pandemic. We have also shown the average experience in 2020-21, for reference, when analysing mortality from these causes; and
- used 2015-21 experience to set our baseline for deaths from all other causes and for coroner-referred deaths, on the basis that it is likely that 2020 and 2021 experience more closely reflects a slow-down in underlying mortality improvement than the impacts of the pandemic.
The baseline for our estimates of excess deaths remains ‘in the absence of the pandemic’ for each of the three years 2020 to 2022. We have not included any COVID-19 deaths in the baseline, as these would not exist in the absence of the pandemic.
As always, it is important to note that predicted death numbers are increasing faster from demographic changes (ageing and population size) than they are reducing due to mortality improvement. Therefore, our model predicts higher baseline numbers of deaths in each successive year.
Baseline Predictions by Age/Gender and State/Territory
For our analysis by age/gender and by state/territory, we have used a slightly different approach as SDRs are not available. Instead, we have scaled the actual deaths in past years to allow for population growth and changes in age mix and have then fitted our linear regression models. As such, our approach is more approximate than if SDRs had been available. Note that our models use annual population changes/adjustments, whereas the ABS uses quarterly estimates of the resident population when calculating SDRs.
We have trained the regression models to the 2015-19 experience to set the baseline for each of the 2020, 2021 and 2022 predicted years.
As for our cause of death models, the baselines for our estimates of excess deaths remain ‘in the absence of the pandemic’ for each of the three years 2020 to 2022.
Given the slight difference of approach, we end up with small differences in the total predicted numbers of deaths from our cause, age/gender and state/territory models.
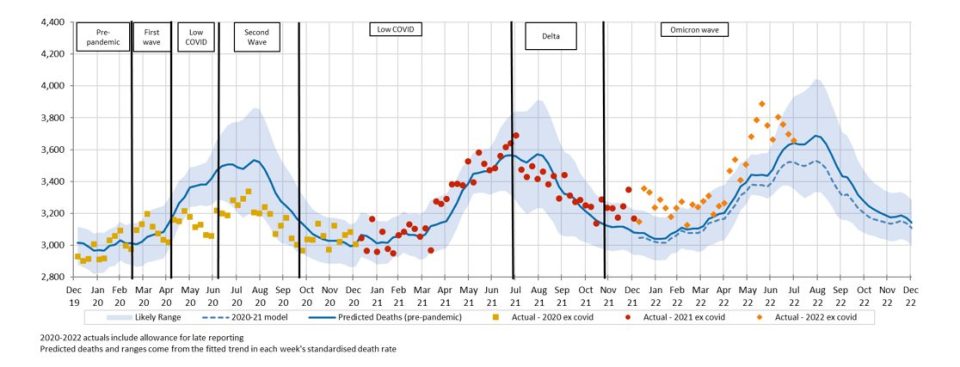
Figure 1 compares the three projections.
(Figure 1 – Weekly predicted deaths – Comparison of Predicted Deaths)
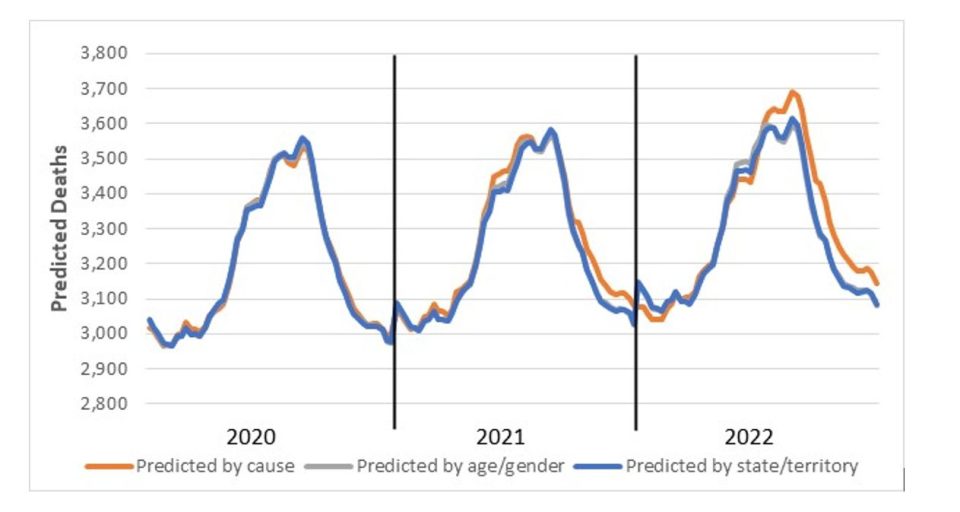
The three different models give very similar results for 2020, with increasing deviation as the projection period extends.
While the predicted values for the age/gender and state/territory models are very similar, our models by cause remain the base for our “best estimate” of total excess mortality, as we believe that they best reflect the underlying mortality trends in Australia.
Comparison with ABS reporting
The results we present here differ from those quoted by the ABS in its commentary surrounding the release of the Provisional Mortality Statistics. For 2022, the most significant difference is in the determination of the baseline, where the ABS uses a simple average of the number of deaths from 2017, 2018, 2019 and 2021, with no allowance for mortality trends or demographic changes. In our view, this understates the baseline and therefore overstates the measure of excess deaths.
For example, the ABS has reported that 18,671 (17.0%) excess deaths occurred by 31 August 2022, in comparison with our estimate of 15,400 (13%).
Excess deaths to 31 August 2022
Figure 2 shows the results of our analysis, comparing actual deaths each week to our predicted values and the 95th percentile prediction interval.
(Figure 2 – Weekly actual and predicted deaths – All Causes)
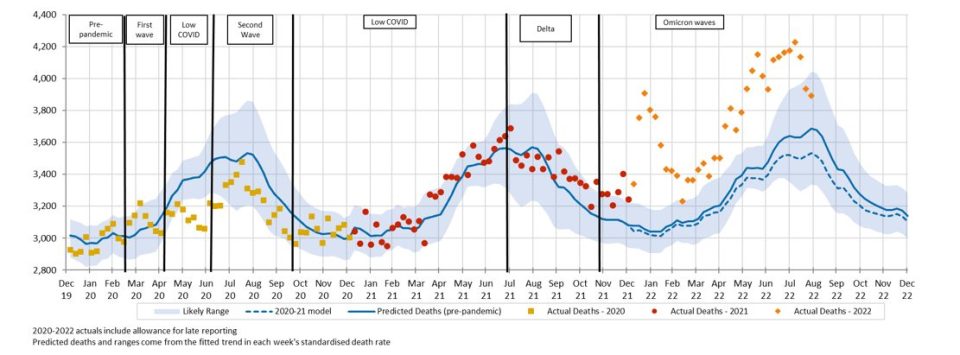
Deaths in the first two new weeks of data (August 2022) were again well above the upper end of the prediction interval (i.e. above the 97.5th percentile), and the second two weeks were at the upper end of the prediction interval. Only three weeks of 2022 have been within the prediction interval, and even these have been at the upper end of that interval.
Figure 3 shows deaths from COVID-19 and with COVID-19, noting that weekly data for with COVID-19 deaths is only available for 2022 and only until the end of July.
(Figure 3 – Weekly actual and predicted deaths – Deaths From and With COVID-19)
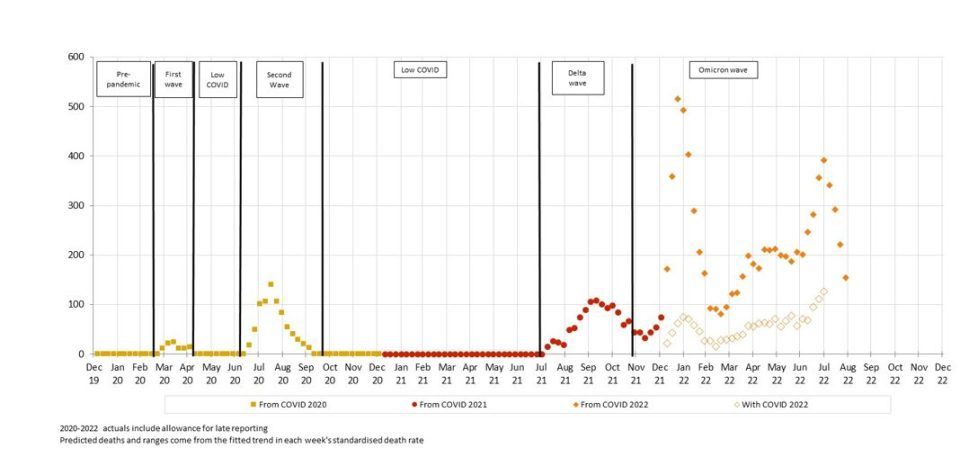
Deaths from COVID-19 peaked in the last week of July and have fallen in each successive week of August.
It is unclear how many people who died with COVID-19 would have died during this period anyway, and how many may have had their death hastened by COVID-19. However, given that with COVID-19 deaths follow the same peaks and troughs as from COVID-19 deaths, it seems that COVID-19 is a catalyst for with COVID-19 deaths, rather than being merely coincidental. We note that the same traditionally happens with the winter peak of respiratory disease deaths.
There may be instances where it is difficult to determine whether a death is due to COVID-19 versus COVID-19 being a contributing cause, and an element of professional judgment by the certifier will necessarily need to be exercised. It is unclear to us how often such decisions may need to be made, and how much “blurring” there may be between from COVID-19 and with COVID-19 deaths.
Figure 4 shows the comparison of actual deaths to predicted after removing from and with COVID-19 deaths. As we are unable to remove with COVID-19 deaths from the four weeks of August, we have not included these points.
(Figure 4 – Weekly actual and predicted deaths – All Causes excluding deaths from and with COVID-19)
Even after removing all from and with COVID-19 deaths, significant excess mortality remains for 2022, with a spike around the time of the January peak in COVID-19 deaths and another coinciding with the peak of the flu season in June/July.
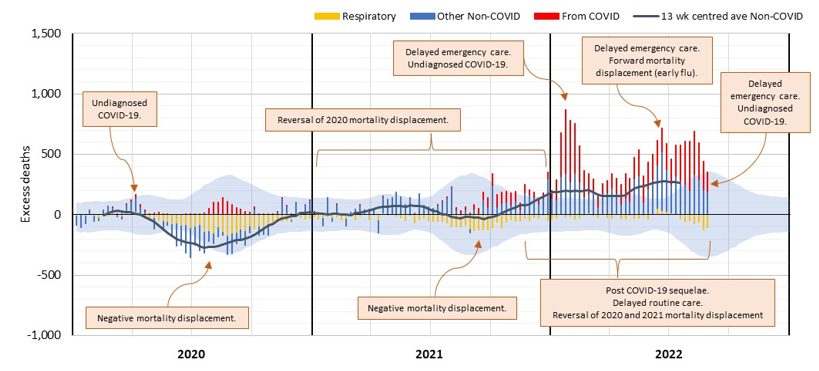
(Figure 5 – Weekly excess deaths – All Causes)
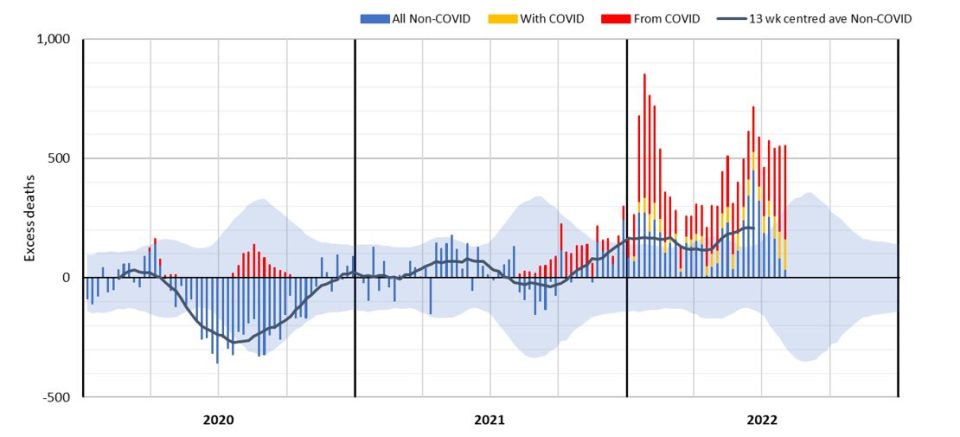
This can be seen clearly in Figure 5, where we divide excess deaths into those from COVID-19, those with COVID-19 and the residual excess from other causes, set against the 95th percentile prediction interval. The increasing trend of non-COVID-19 excess deaths can be seen in the 13-week centred rolling average. The next section discusses the causes of death driving this trend.
Excess deaths to 31 August 2022 by Cause of Death
Table 1 shows our estimate of excess deaths broken down by cause.
As in our previous work, we have assumed that coroner-referred COVID-19 deaths will be 5% of all COVID-19 deaths in 2022, based on the experience of late 2021. If our estimate of coroner-referred COVID-19 deaths is too high (or low), this will not affect the total level of excess deaths measured; it will just mean that our estimate of non-COVID-19 coroner-referred deaths will be too low (or high) by the same amount.
(Table 1 – Excess deaths in Australia – By Cause of Death)
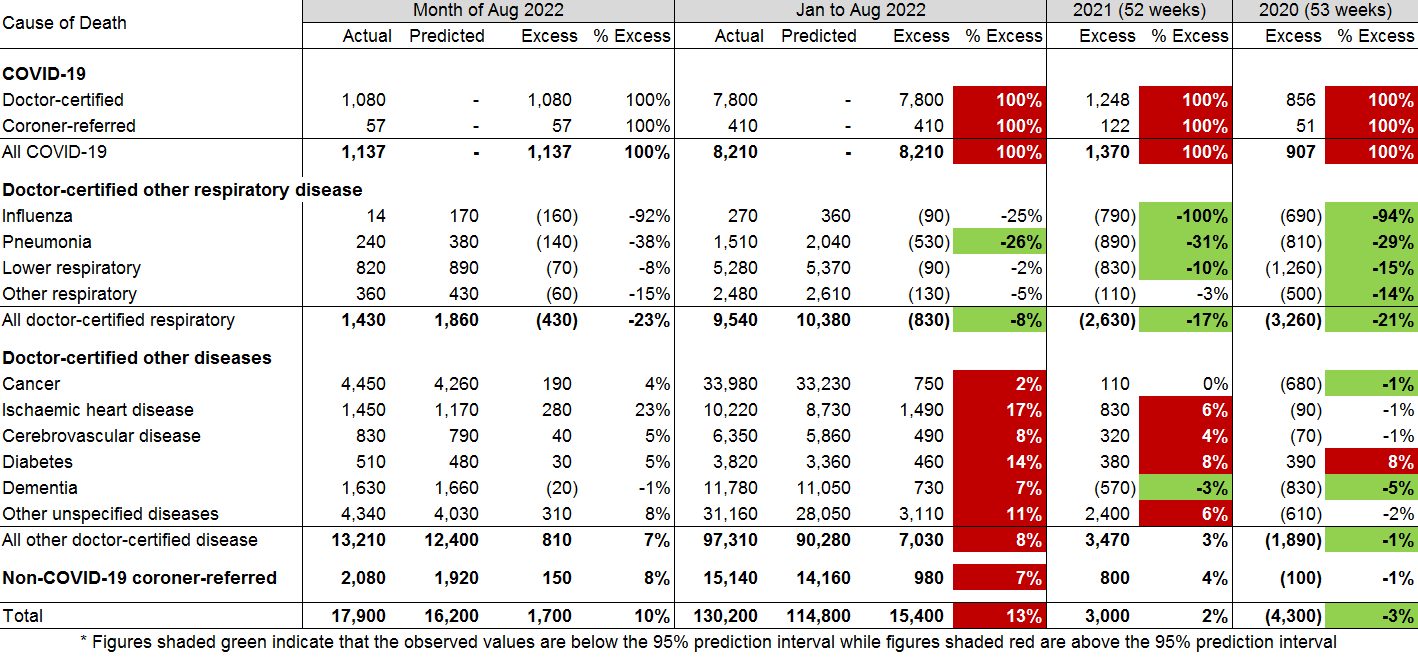
For the month of August 2022:
- Total deaths were 10% (or +1,700) higher than predicted;
- Around two thirds of the excess deaths were due to COVID-19;
- There were far fewer respiratory deaths in August than predicted, reflecting the earlier-than-normal end to the flu season;
- Deaths from ischaemic heart disease were well above predicted; and
- While deaths from dementia were close to predicted, all other causes were in the range 4% to 8% above predicted.
For the first eight months of 2022:
- Total deaths were 13% (or +15,400) higher than predicted, compared with excess deaths of -4,300 for 2020 and +3,000 for 2021;
- There were 8,210 deaths from COVID-19, representing 53% of the excess deaths and including 147 deaths reported as due to Long Covid;
- While not shown in the table, 2,113 deaths with COVID-19 are included among the other causes of death, representing a further 14% of the excess deaths and meaning that 33% of excess deaths (c. 5,000) have no mention of COVID-19 on the death certificate;
- Doctor-certified deaths from respiratory disease continue to be lower than expected (8% lower);
- While doctor-certified deaths from cancer are close to expected in percentage terms (2% higher), this difference is statistically significant;
- Doctor-certified deaths from heart disease, cerebrovascular disease, diabetes and dementia were all significantly higher than predicted (by between 8% and 17%);
- Doctor-certified deaths from other unspecified diseases were also significantly higher than predicted (by 11%), continuing a trend observed since April 2021. Note that this is a large “catch-all” category and it is difficult to infer the reason for this large increase, although history suggests that non-ischaemic heart diseases probably make up around 25% of deaths from other unspecified causes; and
- Non-COVID-19 coroner-referred deaths were 7% higher than expected.
Figure 6 and Figure 7 show weekly excess deaths by underlying cause (thus including deaths with COVID-19) since the start of the pandemic, compared with the 95th percentile prediction interval. All graphs are shown using the same y-axis to give a sense of the contribution of each cause. The 13-week centred average is also shown, to highlight any trends.
(Figure 6 – Weekly excess deaths in 2020-22 for cancer, heart, stroke, and diabetes)
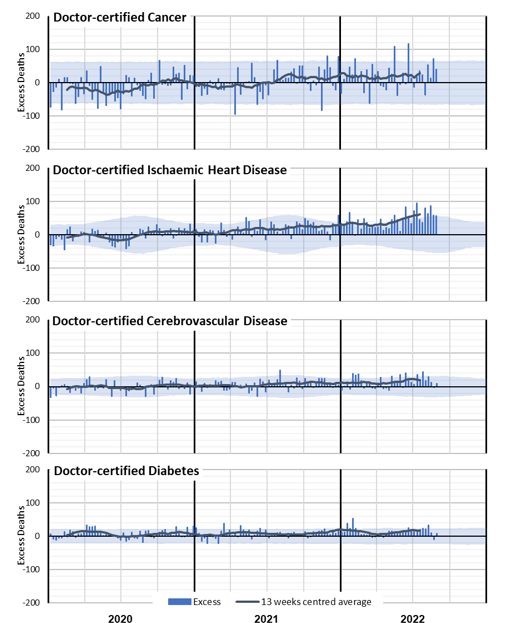
Figure 6 shows a clear increase in excess deaths due to ischaemic heart disease, with increasing trends in cancer and cerebrovascular disease. Diabetes deaths have generally been higher than expected throughout the pandemic. Of these causes, ischaemic heart disease is the biggest contributor to excess deaths in 2022, followed by cancer.
(Figure 7 – Weekly excess deaths in 2020-22 for other causes)
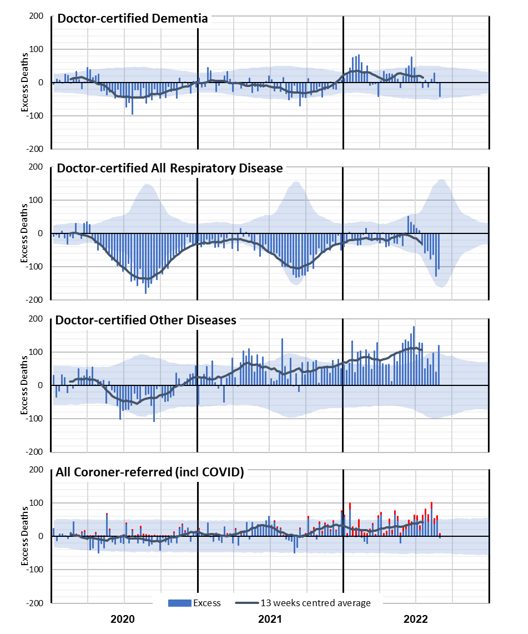
Figure 7 shows negative excess deaths for dementia in 2020 and 2021 (closely correlated with lower respiratory disease) followed by an increasing trend in excess deaths in 2022 (closely correlated with COVID-19 and flu waves). Deaths from respiratory disease have been significantly lower than expected throughout the pandemic, except for the short (and early) flu season in June/July 2022. This coincides with the second 2022 peak in excess non-COVID-19 deaths that we saw in Figure 4 and Figure 5.
Deaths from other diseases (where available ABS data does not specify the cause) were also lower than predicted in 2020 (correlated with lower respiratory disease) but have been, as a group, the largest contributor to non-COVID-19 excess deaths in 2021 and 2022. It is not clear what might be driving this, although we expect that at least part of the excess will be in respect of people who otherwise may have succumbed to respiratory disease in 2020 and 2021.
Coroner-referred deaths include deaths from COVID-19. In Figure 7, we have separately estimated these (in red), based on our estimate that 5% of all COVID-19 deaths are referred to the coroner. The residual non-COVID-19 coroner-referred deaths are well above expected levels in the second half of 2021 and throughout 2022. We note, however, that suicide monitoring reports for NSW and Victoria do not show a marked increase in suicides in those states. Similarly, Australia-wide road death statistics show no major increase.
Excess deaths to 31 July 2022 by Age/Gender
In this section, we discuss figures up to the end of July 2022, rather than August, as we only have COVID-19 deaths by age band up to the end of July.
Table 2 below shows our estimate of excess deaths to the end of July 2022. We have shown the excess including all deaths, and then again after deducting from and with COVID-19 deaths.
(Table 2 – Excess deaths in Australia – By Age/Gender)
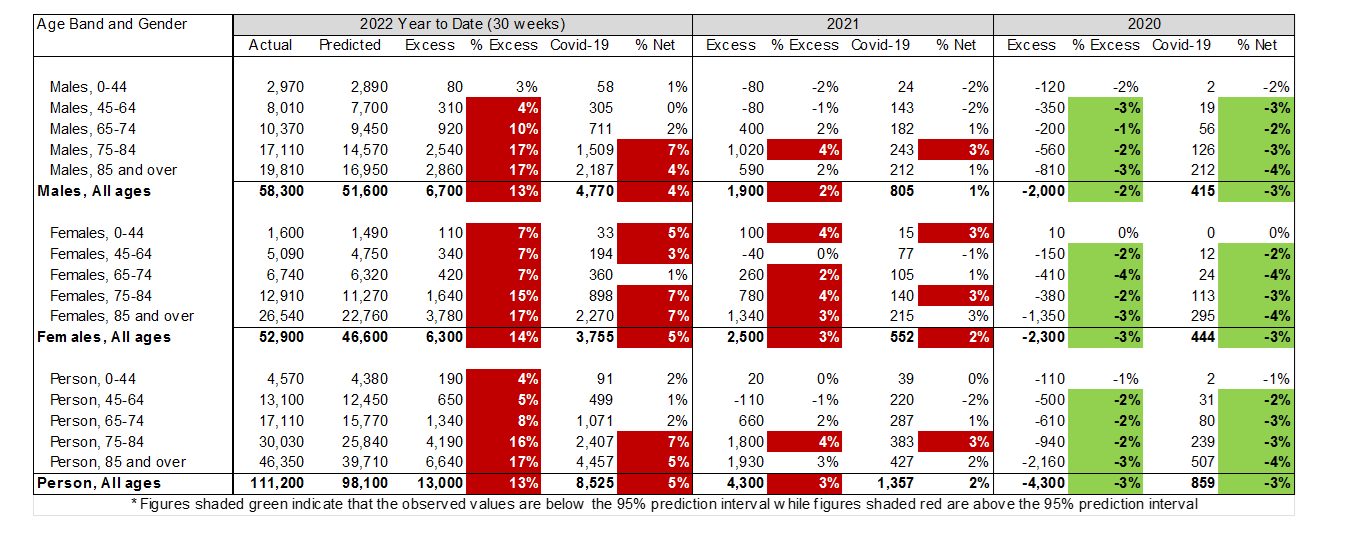
In 2020, all age bands other than the youngest group (0-44 years) had significantly better experience than predicted, even before removing COVID-19 deaths. This is to be expected, as most of the negative excess arose from the lack of respiratory disease and there are very few such deaths in the younger end of the population.
In 2021, females had higher excess mortality than males, but this disparity mostly disappeared after removing COVID-19 deaths. Both males and females aged 75-84 had significant non-COVID-19 deaths, as did females aged 0-44.
Almost all age bands show excess deaths in 2022 (which is not all that surprising given the excess deaths for the whole population), but the number and percentage of excess deaths is higher in older age bands. The risk of mortality from COVID-19 is steeper than the underlying age mortality curve, so this result is somewhat expected.
However, it is notable that there are excess deaths in all age groups and that this excess is generally significant, even after removing COVID-19 deaths. To look at this further, we have shown these results similarly to the graphs by cause, showing weekly excess deaths by age band since the start of the pandemic. For these charts, we have been able to show the contribution of deaths from and with COVID-19 (in orange) separately to non-COVID-19 deaths. The 95th percentile prediction interval is also shown. All age bands are shown using the same y-axis to give a sense of contribution of each age band.
(Figure 8 – Weekly excess deaths in 2020-22 by age band (all persons))
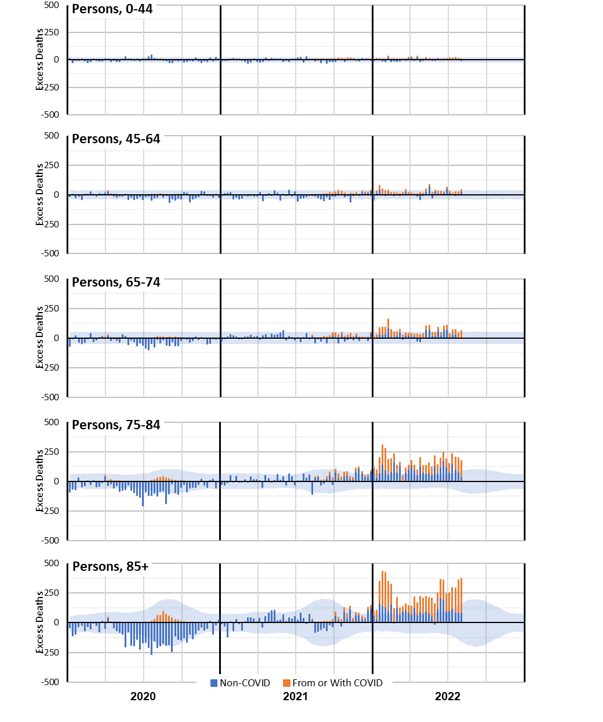
Figure 8 shows that excess deaths in 2022 are dominated by the older age groups. However, we expect many more deaths in these age groups. It is instructive to consider the same information with the excess deaths expressed as a percentage of predicted deaths.
(Figure 9 – Weekly excess deaths as a % of predicted in 2020-22 by age band (all persons))
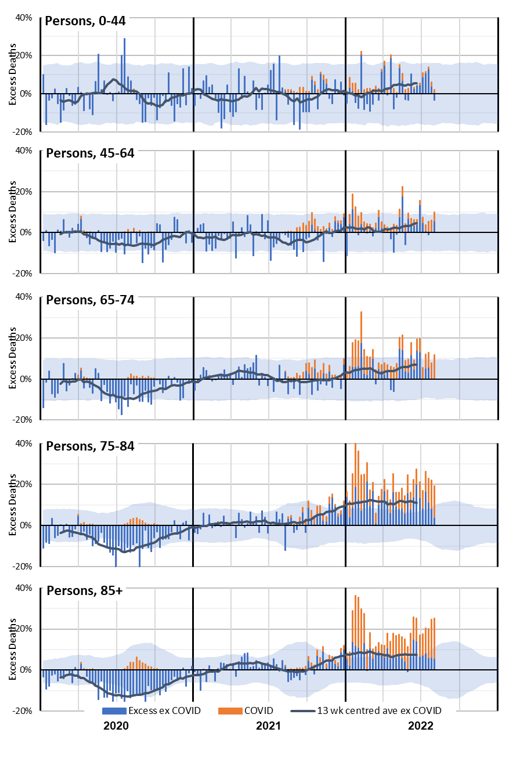
Figure 9 shows that the older ages still experienced the most significant increase in excess deaths when expressed as a percentage of predicted deaths. Indeed, there are very few weeks in 2022 when deaths over the age of 65 are not significantly higher than expected.
While the numbers of deaths in the 0-44 and 45-64 age bands are small, we saw in Table 2 that year-to-date excess deaths in 2022 are materially higher than expected. That table also showed that the percentage excess was higher for females than for males. The differences are worth investigation, although the small numbers mean that there is considerable natural variation.
(Figure 10 – Weekly excess deaths as a % of predicted in 2020-22 for ages 0-44 and 45-64 by gender)
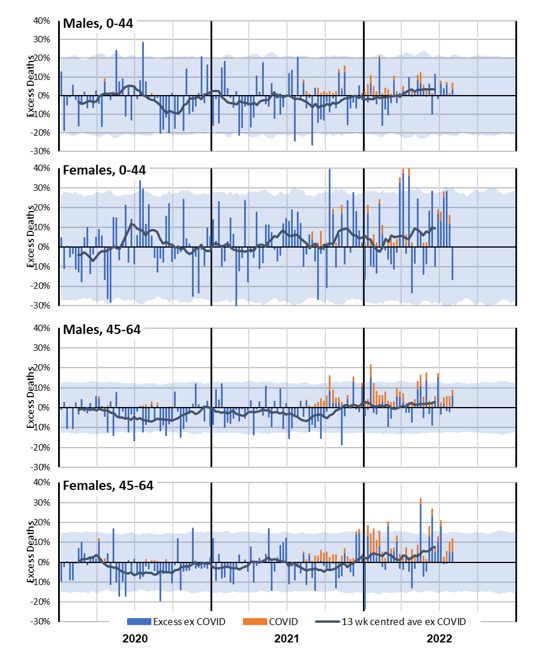
Figure 10 shows that female non-COVID-19 mortality experience in 2021 and 2022 is noticeably worse than male, especially in the 0-44 age band.
Excess deaths to 31 July 2022 by State/Territory
In this section, we discuss figures up to the end of July 2022, rather than August, as we only have COVID-19 deaths by state/territory up to the end of July – and those are limited to deaths from not with COVID-19.
For the first time, this monthly report looks at the breakdown of excess deaths by state/territory. Table 3 shows our estimate of excess deaths to the end of July 2022, before and after deducting deaths from COVID-19.
(Table 3 – Excess deaths in Australia – By State/Territory)
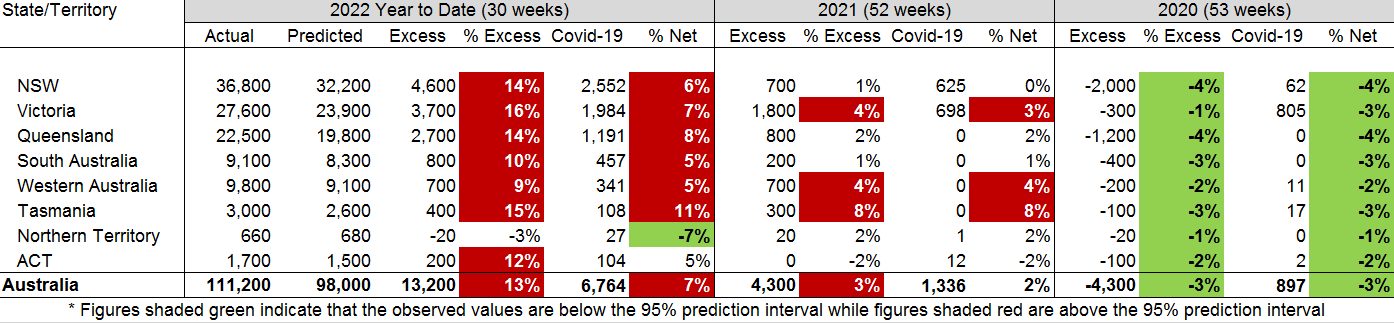
In 2020, all states/territories had similar levels of excess mortality other than Victoria. This is explained by deaths from COVID-19 during the second wave; after deducting deaths from COVID-19, all states/territories had similar – and significant – levels of negative excess mortality.
In 2021, Victoria, Western Australia and Tasmania all had significant levels of excess mortality which were not explained by deaths from COVID-19. The other states/territories all experienced mortality that was not significantly different from predicted.
In 2022, all states/territories apart from NT had significant levels of excess mortality. Generally, about half of this is due to deaths from COVID-19, with the exception of Tasmania.
The lower measured excess mortality for WA reflects the later introduction of widespread COVID-19 into the WA population than in the eastern states.
The graphs below show these results week-by-week for the larger states followed by the smaller states/territories (with the excess shown as a percentage of the predicted value).
(Figure 11 – Weekly excess deaths as a % of predicted in 2020-22 for NSW, Victoria, Queensland, SA and WA)
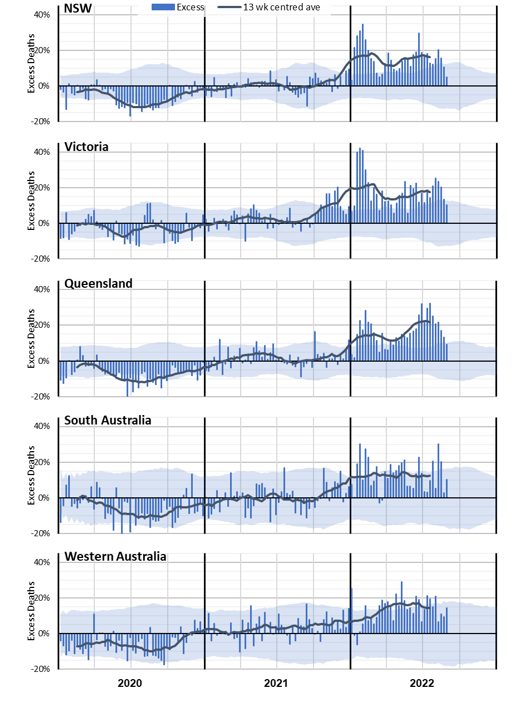
Figure 11 shows that these larger states all had better-than-expected mortality in 2020. It also shows the impact of the second COVID-19 wave in Victoria.
In 2021, Victoria shows a much higher level of excess deaths in the Delta wave – in the last quarter of the year – than other states. Western Australia, while mostly having excess deaths within the 95th percentile prediction interval, had many more weeks with positive excess deaths than with negative excess deaths.
In 2022, the experience of the three largest states is similar, although Queensland’s second peak in 2022 is larger than the first. SA is also similar, although somewhat more volatile given its smaller size. In WA, there is an absence of a large COVID-19 spike in January/February due to its border closure.
(Figure 12 – Weekly excess deaths as a % of predicted in 2020-22 for Tasmania, ACT and NT)
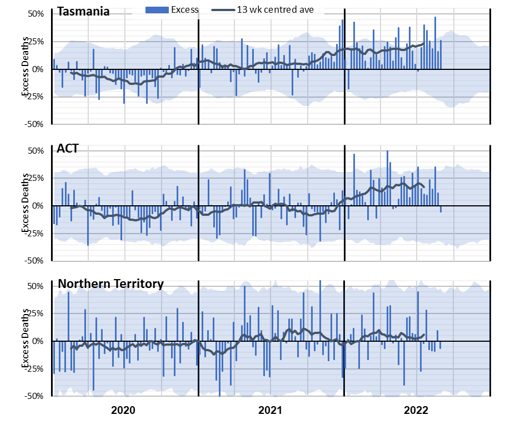
Figure 12 shows the higher volatility of excess mortality experienced by the smallest state and the two territories. Allowing for that volatility, Tasmania had broadly the same experience of excess mortality as the larger states, but with a high level of excess deaths during the Delta wave late in 2021.
With its relatively young and affluent population, the ACT has experienced lower excess mortality than the larger states.
The Northern Territory has a very young population, which might explain the low net impact of the pandemic after allowing for the high volatility caused by a very small weekly expected death count. There is no apparent trend in the excess mortality.
Figure 13 shows the excess deaths by month for 2022, with deaths from COVID-19 shown separately from other causes (with COVID-19 deaths are not available and are included with deaths from other causes).
(Figure 13 – Monthly excess deaths as a % of predicted in 2022 for the six states)
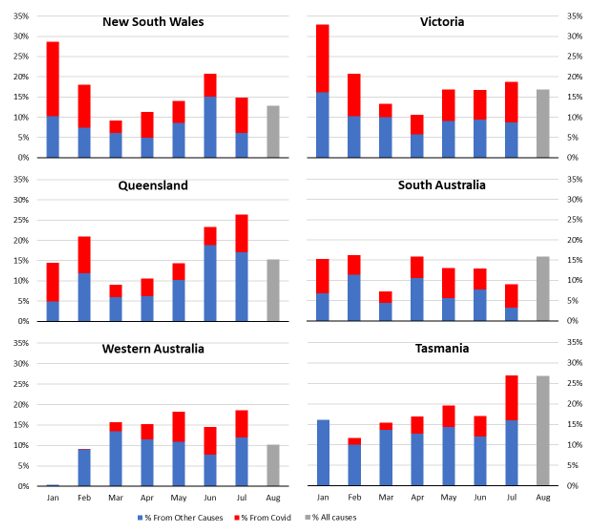
Once again, the WA picture is quite different, with very few excess deaths in January 2022, no COVID-19 deaths in January and very few in February. Tasmania has relatively fewer from COVID-19 deaths than the other states.
What could be causing the non-COVID-19 excess deaths?
The measurement of higher numbers of deaths than predicted does not tell us why this is occurring. There are several reasons hypothesised around the world (where this effect is occurring to a greater or lesser extent). It isn’t possible to identify from death counts alone what is causing the non-COVID-19 excess deaths, but we have listed below the most likely explanations. We note that multiple factors are likely in play, and different factors may be more or less pronounced at various times.
To summarise the evidence from earlier sections:
- Deaths with COVID-19 have followed the same pattern as deaths from COVID-19 in 2022;
- Non-COVID-19 excess deaths have been highest when there have been peaks in COVID-19 deaths and peaks in influenza deaths;
- Deaths due to some causes (dementia and “other” diseases in particular) are closely correlated to the level of respiratory disease circulating;
- Non-COVID-19 excess deaths are particularly apparent in the oldest two age groups for both genders, and the youngest two age groups for females only;
- Non-COVID-19 excess deaths are less apparent when there is no COVID-19 circulating.
Based on these observations, the following indicates which factors, in our view, are likely to be having a greater or lesser impact on Australian excess mortality in 2022.
- Post-COVID-19 sequelae or interactions with other causes of death: Studies have shown that COVID-19 is associated with higher subsequent mortality risk from heart disease and other causes, but certifying doctors would generally not identify a causative link several months after recovery from COVID-19. Therefore, it seems likely that there would be more of these deaths than identified. The age-based analysis supports this hypothesis, with non-COVID-19 excess deaths occurring in 2022 even in those under 45, noting that this age group has had low levels of COVID-19 deaths. The absence of excess deaths in WA in January also supports this explanation.
Likely impact in Australia: High
- Delay in emergency care: Pressure on the health, hospital and aged care systems, including ambulance ramping and bed block, could lead to people not getting the care they require, either as they avoid seeking help, or their care is not as timely as it might have been in pre-pandemic times. The peaks in non-COVID-19 excess deaths at times of high COVID-19 and/or influenza deaths supports this hypothesis.
Likely impact in Australia: High during COVID-19 and influenza peaks
- Mortality displacement: Australia had negative mortality displacement (i.e. fewer deaths than expected) in the first year or so of the pandemic, resulting from the absence of many respiratory diseases. The lower-than-expected mortality from respiratory disease was again apparent in 2021. As such, some of the excess we have seen in some causes in 2021 and 2022 may be the reversing of this effect. People who otherwise may have died earlier had their systems been stressed by respiratory disease may now be succumbing to their underlying illnesses. Conversely, the earlier-than-usual flu season in 2022 appears to have resulted in some forward mortality displacement.
Likely impact in Australia: Moderate, likely to reduce over time
- Delay in routine care: Opportunities to diagnose or treat non-COVID-19 diseases have been missed for various reasons including fear and lack of opportunity. There is some evidence that this may be affecting cancer deaths. It may also be a factor in higher deaths from other causes, such as ischaemic heart disease, diabetes, and the large “other” category.
Likely impact in Australia: Low to Moderate, likely to increase over time
- Undiagnosed COVID-19: Some of the excess deaths could be from unidentified COVID-19. This effect happened early in the pandemic, but it seems less likely in 2022, as testing is much more available, particularly for those who are seriously ill. Also, for any deaths where COVID-19 may be suspected, post-mortem testing is occurring in Australia. That said, the timing of the higher levels of non-COVID-19 excess deaths (once deaths with COVID-19 are also removed) coinciding with high levels of COVID-19 deaths suggests that there may be some undiagnosed COVID-19 deaths.
Likely impact in Australia: Low, perhaps higher during COVID-19 peaks
- Mental health issues: There has been much discussion throughout the pandemic about the impacts on mental health, including commentary that lockdowns and other measures are causing an increase in suicide deaths. Data from the latest ABS Causes of Death, Australia publication shows that age-standardised suicides rates for both males and females were lower in 2020 and 2021 compared with the preceding three years, noting that the 2020 and 2021 data is preliminary. The publication also shows that 3.2% of suicide deaths in 2020 (0.06% of all deaths) and 2.6% in 2021 (0.05% of all deaths) had the pandemic mentioned as a risk factor. Even where the pandemic was a risk factor, there were, on average, five other risk factors. The suicide monitoring reports for NSW and Victoria show the same picture for 2020 and 2021, with 2022 also unchanged in NSW and up only a little in Victoria. (Lifeline: 13 11 14)
Likely impact in Australia: Low
- Pandemic-influenced lifestyle changes: There is evidence from the UK that a higher proportion of people made less healthy lifestyle choices during lockdowns (e.g. drinking more alcohol, exercising less, higher rates of childhood obesity), and that these less healthy practices have continued. It is unclear to what extent similar factors may be affecting mortality in Australia in 2022. Deaths directly caused by drug and/or alcohol abuse are relatively low, compared with those from other causes, but there would be an indirect impact.
Likely impact in Australia: Low
- Vaccine-related deaths: While there have been deaths in Australia caused by the administration of COVID-19 vaccines, the number of such deaths has been small. Australia has a very good vaccine approval and safety monitoring processes, administered by the Therapeutic Goods Administration. The latest vaccine safety report (to 17 November) shows that, of the 944 reports of death following vaccination, only 14 were found to have been caused by the administration of the vaccine. In addition, the vaccine rollout ramped up slowly from February 2021, with high rates of vaccination in August to October 2021 and again in January 2022, but has been low for most of 2022. This does not fit with the timing or shape of the excess mortality.
Likely impact in Australia: Negligible
Figure 14, which shows excess deaths from doctor-certified respiratory disease, other non-COVID causes and those from COVID-19, puts the above into context, across the pandemic. Note that deaths with COVID-19 are included with the primary non-COVID cause (respiratory or other).
(Figure 14 – Possible causes of non-COVID-19 excess mortality from time to time during the pandemic)
COVID-19 deaths in September to November 2022
While the ABS Provisional Mortality Statistics data is only available up to the end of August 2022, surveillance COVID-19 deaths are available up to the end of November 2022. Figure 15 shows the number of such deaths in each month since January 2020.
Note that, with the change to weekly reporting of COVID-19 surveillance statistics, it is no longer possible to report full calendar months. The months shown are:
- September 2022: 1 September to 29 September (1 September to 27 September for Queensland)
- October 2022: 30 September to 27 October (28 September to 25 October for Queensland)
- November: 28 October to 24 November (26 October to 22 November for Queensland).
(Figure 15 – COVID-19 deaths in Australia, reported from surveillance systems*)
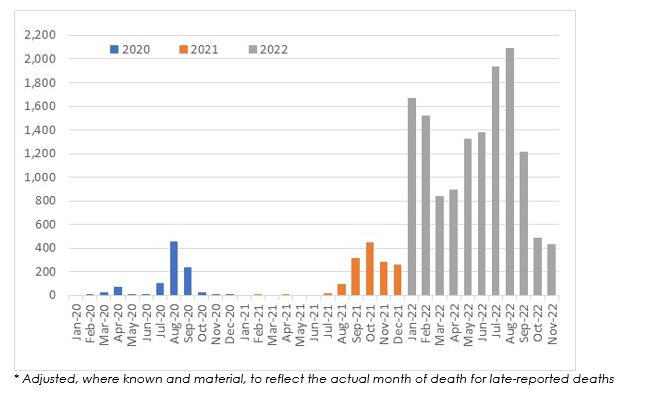
In the eleven months to end November 2022, there have been approximately 13,800 COVID-19 deaths. Of these, around 2,150 occurred in the three months to end November 2022 (where we have no provisional mortality statistics).
The COVID-19 Mortality in Australia article shows the proportion of those death certificates mentioning COVID-19 where COVID-19 was the underlying cause. Figure 16 shows a comparison of deaths from COVID-19 versus those with COVID-19. For the most recent months, a large proportion of deaths have not yet been registered, so we have also shown our estimate of the numbers of as-yet unregistered deaths.
Figure 16 also contains a line showing the proportion of registered COVID-19-related deaths that were from rather than with COVID-19. With many deaths are still to be registered, this point is shown as a preliminary estimate.
(Figure 16 – A comparison of deaths From COVID-19 to those With COVID-19 (source: ABS))
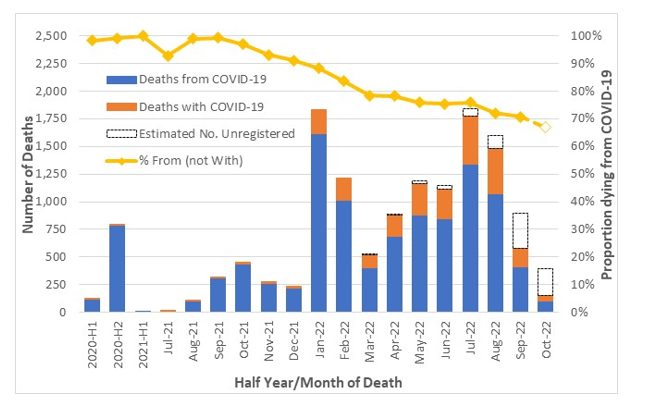
The proportion of registered COVID-19 deaths from COVID-19 has reduced in 2022, from 88% in January, to 75% in May to July, and then a substantial drop to around 70% in August to October.
We consider it reasonable to assume that, of the 2,150 “COVID-19” deaths reported in September to November 2022, 70% may have been from COVID-19 rather than with COVID-19. Therefore, we estimate that around 1,500 deaths in this period may have been due to COVID-19.
Our prediction model suggests that, without a pandemic, there would have been a total of around 43,900 deaths in the three months September to November 2022.
Thus, COVID-19 deaths represent around 3% extra mortality over September to November 2022 (6% in September and 2% in October and November). There have probably continued to be fewer deaths from respiratory diseases in this period than our pre-pandemic predictions. However, we consider it likely that mortality from non-COVID-19, non-respiratory causes will be higher than our pre-pandemic predictions, given the higher-than expected mortality in 2021 and the first eight months of 2022, and that this will outweigh the benefit from respiratory disease. Therefore, we expect that total excess mortality in September to November 2022 will have been higher than the 3% explained by COVID-19.
Standardised Mortality Rates
Figure 17 shows the cumulative standardised mortality rates (SDRs) for 2015 to 2022, expressed relative to the rate for 2019. The SDRs are from the Provisional Mortality Statistics, plus allowance for late-reported deaths.
(Figure 17 – Cumulative standardised mortality rate relative to 2019)
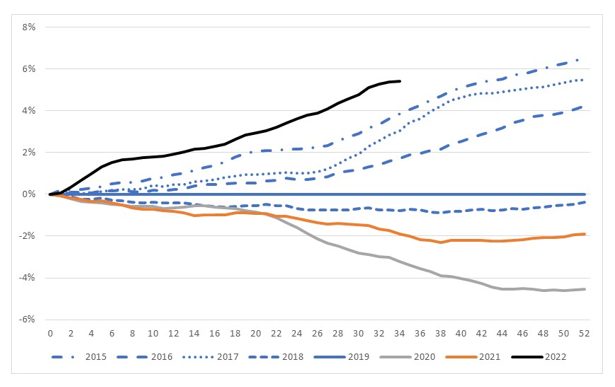
The graph shows that:
- Mortality rates improved over the 2015 to 2019 pre-pandemic years, noting that both 2017 and 2019 were “bad” influenza years, resulting in higher than usual deaths both from and related to influenza;
- The 2020 year is considerably lower than 2019, a result of the lower number of respiratory and respiratory-related deaths in this year due to measures introduced to curb COVID-19;
- 2021 is higher than 2020, a combination of both deaths from COVID-19 during the Delta wave and excess mortality from other causes of death; and
- Experience for the first eight months of 2022 is higher than for any other year shown.
Leading causes of death
For brevity, we have not included our analysis of leading causes of death in this article. We continue to expect that COVID-19 will be the third leading cause of death in 2022.
Disclaimer
We are not medical professionals, public health specialists or epidemiologists. This note is based on publicly available information and our general observations on that data.
COVID-19 Mortality Working Group
The members of the Working Group are:
- Angelo Andrew
- Karen Cutter
- Jennifer Lang
- Han Li
- Richard Lyon
- Zhan Wang
- Mengyi Xu
CPD: Actuaries Institute Members can claim two CPD points for every hour of reading articles on Actuaries Digital.






